Starting hormone replacement therapy after 50 brings significant changes to a woman’s body as it works to restore hormones that naturally decline during menopause. Many women wonder if it’s safe to begin or continue HRT in their fifties and beyond, especially given conflicting information about long-term use.

HRT after 50 can provide relief from menopause symptoms while supporting bone health, heart function, and overall quality of life when started within 10 years of menopause. Research shows that women who start HRT within 10 years of menopause or before age 60[1] tend to experience the most benefits with reduced risks. The therapy works by replacing estrogen and progesterone that the body no longer produces in adequate amounts.
Understanding what happens in the body during HRT treatment helps women make informed decisions about their health. For most women, hormone replacement therapy is a safe and effective option[2] for managing menopause symptoms that can be disabling and last for years. The key lies in choosing the right type of hormones and delivery method based on individual health factors.
Key Takeaways
- HRT restores declining hormones to reduce menopause symptoms and support overall health after 50
- Starting treatment within 10 years of menopause provides the best benefit-to-risk ratio for most women
- The type of hormones and delivery method should be personalized based on individual health needs and risk factors
How HRT Works in the Body After 50
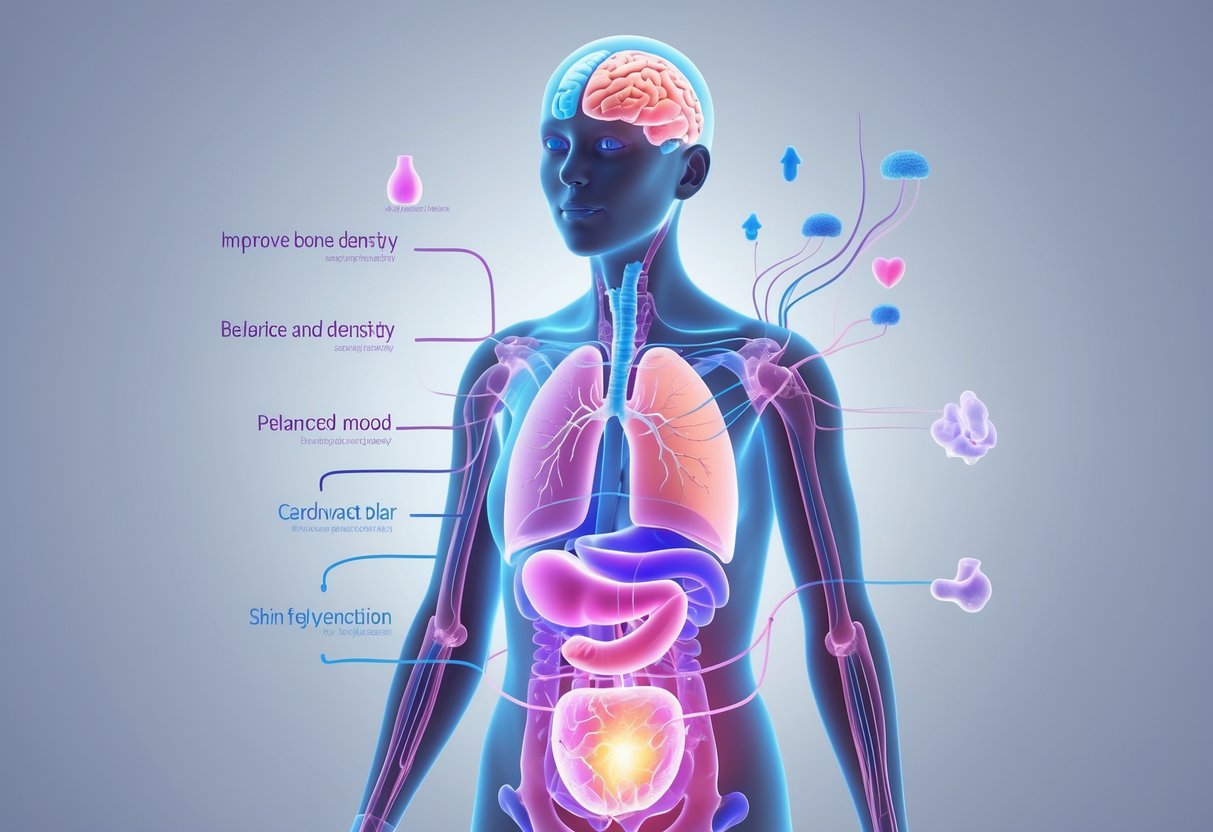
After age 50, hormone replacement therapy works by adding back the estrogen and progesterone that decline during menopause. These hormones affect multiple body systems, from bones and muscles to the heart and brain.
The Role of Estrogen and Progesterone
Estrogen serves as the primary hormone in hormone replacement therapy for postmenopausal women. It binds to estrogen receptors throughout the body to restore normal cell function.
Key functions of estrogen include:
- Maintaining bone density
- Supporting heart health
- Regulating body temperature
- Preserving vaginal tissue
Progesterone balances estrogen’s effects in women who still have their uterus. It protects the uterine lining from overgrowth that estrogen alone can cause.
The delivery method matters significantly[1] for how these hormones work. Oral estrogen passes through the liver first, which can affect cholesterol and triglycerides.
Patches, gels, and sprays deliver hormones directly through the skin. This avoids liver processing and reduces certain risks.
Hormonal Changes After Menopause
Natural hormone production drops sharply during menopause. Estrogen levels fall by 90% or more from peak reproductive years.
This dramatic decline triggers the symptoms women experience:
- Hot flashes and night sweats
- Sleep disruption
- Mood changes
- Vaginal dryness
HRT works by introducing new hormones[3] into the body. It either supplements existing hormones or replaces them entirely based on individual needs.
The timing of treatment affects how well it works. Starting HRT within 10 years of menopause typically provides the best results with lower risks.
Impact on Vital Body Systems
HRT affects multiple body systems simultaneously after age 50. The cardiovascular system responds quickly to restored estrogen levels.
Bone health improvements:
- Increased bone mineral density
- Reduced fracture risk
- Better calcium absorption
Muscle and metabolic changes:
- Maintained muscle strength[4]
- Improved exercise capacity
- Better body composition
The nervous system also responds to hormone replacement. Women often report improved mood, better sleep, and clearer thinking within weeks of starting treatment.
Skin and hair typically improve with HRT. Collagen production increases, leading to better skin elasticity and reduced dryness.
Systemic estrogen therapy[5] comes in pills, patches, rings, gels, creams, or sprays. Each method delivers different hormone levels throughout the body.
Key Benefits of HRT for Women Over 50

HRT provides targeted relief for three major health challenges women face after 50. The therapy addresses uncomfortable vasomotor symptoms like hot flashes, protects against bone loss that accelerates after menopause, and restores vaginal and urinary tissue health.
Relief of Menopausal Symptoms
Hot flashes affect up to 80% of women during menopause and can persist for years. These vasomotor symptoms disrupt daily life and sleep quality.
HRT effectively relieves most perimenopause and menopause symptoms[6], including hot flashes and night sweats. Women typically notice improvement within 4-6 weeks of starting treatment.
Common symptoms HRT addresses:
- Hot flashes (frequency reduced by 75-80%)
- Night sweats
- Sleep disturbances
- Mood changes
- Brain fog
The therapy works by replacing estrogen levels that drop sharply during menopause. This hormone replacement helps regulate the body’s temperature control system.
Many women experience complete elimination of hot flashes within three months. Night sweats often improve even sooner, leading to better sleep quality and daytime energy levels.
Bone Health and Osteoporosis Prevention
Women lose up to 20% of their bone density in the first five years after menopause. This rapid bone loss increases fracture risk significantly.
Evidence suggests HRT protects bones[7] by slowing the breakdown process that accelerates when estrogen levels drop. The therapy helps maintain bone mineral density in the spine and hips.
Key bone benefits include:
- Reduced fracture risk by 30-40%
- Preserved spine density
- Maintained hip bone strength
- Slower overall bone loss
HRT works best for bone protection when started within 10 years of menopause. The therapy prevents the rapid bone loss phase that occurs immediately after estrogen production stops.
Women who use HRT for five years or more show significantly better bone density compared to those who don’t receive treatment. This protection continues as long as therapy continues.
Support for Vaginal and Urinary Health
Estrogen keeps vaginal and urinary tissues healthy and flexible. Without it, these tissues become thin and dry, causing discomfort and infections.
Estrogen eases vaginal symptoms of menopause[8], including dryness, itching, burning and pain during intercourse. It also helps with bladder symptoms that develop after menopause.
Vaginal and urinary improvements:
- Restored natural lubrication
- Reduced burning and itching
- Less painful intercourse
- Fewer urinary tract infections
- Improved bladder control
Vaginal estrogen can be applied directly to the area for targeted treatment. This local therapy provides relief without affecting hormone levels throughout the body.
Women often notice vaginal improvements within 2-3 weeks of starting treatment. Urinary symptoms may take slightly longer to improve but typically respond well to consistent therapy.
Potential Risks and Side Effects
While HRT offers many benefits for women over 50, it does carry some health risks that require careful consideration. Recent evidence shows that risks of serious side effects from HRT are very low[4], but understanding breast cancer risks, blood clot formation, and cardiovascular effects helps women make informed decisions about treatment.
Breast Cancer Considerations
HRT can slightly increase breast cancer risk, particularly with combined estrogen and progestin therapy. Studies show around 5 extra cases of breast cancer occur in every 1,000 women who take combined HRT for 5 years[4].
The risk increases with longer treatment duration and older age. It decreases after stopping HRT.
Estrogen-only HRT carries little to no increased breast cancer risk. This option is available for women who have had hysterectomies.
Risk factors that matter:
- Length of treatment
- Type of HRT used
- Individual health history
- Age when starting treatment
Women with previous breast cancer typically cannot use HRT. Regular mammogram screenings become especially important for women taking hormone therapy.
Blood Clots and Stroke
HRT affects blood clot and stroke risk differently depending on the delivery method. HRT tablets can increase blood clot risk, while patches, sprays and gels do not increase this risk[4].
Oral HRT carries higher risks because hormones pass through the liver first. This process increases clotting proteins in the blood.
Transdermal HRT (patches, gels, sprays) bypasses the liver. Estrogen absorbed through skin does not trigger the same clotting response.
Stroke risk increases slightly with oral HRT but remains very low, especially for women under 60. The absolute risk stays minimal for most healthy women.
Women at higher risk for blood clots typically receive non-oral HRT forms. Risk factors include obesity, smoking, family history, and previous clotting episodes.
Heart Health and Coronary Artery Disease
HRT’s effects on heart health depend heavily on timing and individual risk factors. Research shows that taking HRT has little or no effect on coronary heart disease risk[4].
Starting HRT within 10 years of menopause may provide heart protection. Beginning treatment many years after menopause can increase cardiovascular risks.
The WHI study initially raised concerns about heart disease risks. However, newer analysis shows these risks primarily affected older women who started HRT years after menopause.
Heart-healthy HRT use involves:
- Starting within 10 years of menopause
- Using appropriate doses
- Regular medical monitoring
- Considering individual risk factors
Women with existing heart disease need specialized evaluation before starting HRT. The timing of treatment initiation significantly influences cardiovascular outcomes.
Types of HRT and Administration Methods

HRT comes in different hormone combinations and delivery methods to meet individual needs. Women can choose between estrogen-only treatments or combined therapies, with options for daily continuous dosing or cyclical patterns that mimic natural hormone cycles.
Estrogen-Only HRT
Estrogen-only HRT is recommended for women who have had their womb removed[9] during a hysterectomy. Without a uterus, women don’t need progesterone to protect against endometrial cancer.
This therapy replaces the estrogen that declines during menopause. It helps reduce hot flashes, night sweats, and vaginal dryness.
Common delivery methods include:
- Daily tablets
- Skin patches changed every few days
- Gels applied to skin once daily
- Nasal sprays
- Vaginal rings
Women take estrogen-only HRT continuously without breaks. The dosage stays consistent throughout the month.
Combined Estrogen and Progesterone Therapy
Women who still have their uterus need both estrogen and progestogen to protect against womb cancer[9]. The progesterone component prevents the uterine lining from growing too thick.
Combined therapy comes as single medications containing both hormones. Women can also take separate estrogen and progesterone products.
Progesterone sources include:
- Oral tablets taken daily
- Mirena IUD that releases hormones for up to 5 years
- Vaginal gels or suppositories
The combination addresses multiple menopause symptoms. It maintains bone density and reduces cardiovascular risks when started early in menopause.
Sequential vs. Continuous HRT
Sequential HRT mimics natural menstrual cycles. Women take estrogen daily and add progesterone for 10-14 days each month. This causes monthly withdrawal bleeding.
Sequential combined HRT works best for women still having periods[9] during perimenopause. The cycling prevents breakthrough bleeding between periods.
Continuous HRT provides steady hormone levels without breaks. Women take both estrogen and progesterone daily. This stops monthly bleeding completely.
Continuous combined HRT suits women who haven’t had periods for over one year[9]. It eliminates monthly withdrawal symptoms and bleeding.
| Sequential HRT | Continuous HRT |
|---|---|
| Monthly bleeding occurs | No bleeding expected |
| Best for perimenopause | Best for postmenopause |
| Hormone levels fluctuate | Steady hormone levels |
Local Hormone Therapies
Vaginal estrogen treats local symptoms without affecting the whole body[9]. It comes as creams, tablets, rings, or gels inserted into the vagina.
This low-dose treatment helps with vaginal dryness, burning, and painful intercourse. It doesn’t increase breast cancer risk like systemic HRT.
Local estrogen products:
- Vaginal creams applied 2-3 times weekly
- Vaginal tablets inserted twice weekly
- Flexible rings replaced every 3 months
- Vaginal gels used as needed
Vaginal estrogen can be used safely even by women with a uterus[9] without needing progesterone. The hormone stays localized and doesn’t significantly enter the bloodstream.
Women can use local treatments alone or combine them with systemic HRT. This dual approach addresses both whole-body and vaginal symptoms effectively.
Psychological and Cognitive Effects

HRT can significantly impact mental health and brain function after age 50, with effects on mood stability, anxiety levels, and cognitive performance. Sleep quality often improves, which supports overall psychological well-being.
Mood Changes and Anxiety
HRT helps stabilize mood swings that occur during menopause and postmenopause. Many women experience fewer episodes of irritability and emotional ups and downs.
Anxiety reduction is one of the most notable benefits. Estrogen helps regulate neurotransmitters like serotonin, which directly affects anxiety levels.
Some women may still need additional support through selective serotonin reuptake inhibitors (SSRIs) alongside HRT. The combination can be more effective than either treatment alone.
Depression symptoms often improve within the first few months of starting HRT. This happens because hormones help restore chemical balance in the brain.
Women who experienced severe mood changes during menopause typically see the most dramatic improvements. The psychological effects of HRT[10] extend beyond just managing physical symptoms.
Cognitive Health and Dementia
HRT may protect brain function when started around the time of menopause. Estrogen supports memory formation and helps maintain thinking skills.
Memory improvements are common in the first year of treatment. Many women report better word recall and clearer thinking.
The timing of HRT matters greatly for cognitive benefits. Starting treatment within five years of menopause appears most protective against cognitive decline.
Research shows mixed results about dementia prevention. Some studies suggest reduced risk of Alzheimer’s disease[11] with early HRT use, while others show no long-term protection.
Attention and focus often improve as menopausal symptoms decrease. Brain fog, a common complaint during menopause, typically clears within months of starting treatment.
Sleep Quality and Well-being
Better sleep is one of the fastest improvements women notice on HRT. Fewer night sweats and hot flashes lead to more restful sleep.
Sleep disturbances that cause mood changes and cognitive difficulties often resolve quickly. This creates a positive cycle of better rest and improved mental health.
Deep sleep phases become longer and more consistent. This helps with memory consolidation and emotional regulation.
Many women report feeling more energetic during the day. Better sleep quality directly impacts mood stability and reduces anxiety levels.
Overall well-being improves as sleep patterns normalize. The connection between hormone therapy and improved sleep[12] supports better psychological health across all areas.
Personalizing HRT: Factors to Consider
The decision to start HRT requires careful evaluation of individual circumstances, timing, and health status. Age at initiation, personal medical history, and commitment to lifestyle modifications all play crucial roles in determining treatment success and safety.
Age and Timing of Initiation
Starting HRT closer to menopause onset provides the most benefits with lower risks. Research shows that women under 60 years old who begin treatment within 10 years of menopause[13] have significantly better outcomes than those who start later.
Women in their 40s and 50s experience fewer complications compared to those who begin after age 60. The body’s tissues remain healthier when treatment starts soon after hormone levels begin declining naturally.
Optimal timing windows:
- Early menopause (under 50): Immediate benefits with minimal risks
- Natural menopause (50-55): Best risk-to-benefit ratio when started within 2 years
- Late initiation (over 60): Higher risks may outweigh potential benefits
The timing principle applies because blood vessels and other tissues respond better to hormone replacement when they haven’t been without estrogen for extended periods.
Medical History and Individual Risk
Personal and family medical history significantly influences HRT safety and effectiveness. Women with certain conditions may face higher risks or need modified treatment approaches.
Higher risk conditions include:
- History of blood clots or stroke
- Breast or ovarian cancer history
- Active liver disease
- Unexplained vaginal bleeding
Type 2 diabetes requires special consideration, as HRT can affect blood sugar control and metabolism. Some women with diabetes may benefit from improved insulin sensitivity, while others need closer monitoring.
Healthcare providers must evaluate each woman’s unique risk factors[7] before recommending treatment. Family history of heart disease, osteoporosis, and hormone-sensitive cancers all factor into the decision-making process.
Previous pregnancy complications, current medications, and smoking status also influence treatment recommendations and monitoring requirements.
Lifestyle Changes and Healthy Habits
A healthier lifestyle enhances HRT effectiveness and reduces potential risks. Women who maintain good health habits typically experience better outcomes and fewer side effects.
Key lifestyle changes include:
- Regular exercise (150 minutes weekly)
- Balanced nutrition with adequate calcium and vitamin D
- Smoking cessation
- Limited alcohol consumption
- Stress management techniques
These modifications support healthy metabolism and can reduce the risk of complications like blood clots and stroke. Exercise particularly helps maintain bone density and cardiovascular health during treatment.
Diet changes that emphasize whole foods, lean proteins, and plenty of fruits and vegetables support optimal hormone metabolism. Weight management becomes especially important, as excess weight can increase certain HRT risks.
Follow-up and Monitoring
Regular monitoring ensures HRT remains safe and effective throughout treatment. Healthcare providers typically schedule appointments every 3-6 months initially, then annually for stable patients.
Monitoring includes:
- Blood pressure checks
- Breast and pelvic examinations
- Mammograms and bone density scans
- Blood tests for liver function and cholesterol
Women should report any unusual symptoms, including breast changes, leg swelling, or severe headaches. These could indicate complications requiring immediate attention or treatment adjustments.
Treatment plans should be reviewed regularly[8] to ensure they continue meeting individual needs. Dose adjustments, delivery method changes, or treatment discontinuation may become necessary based on ongoing health status and symptom management.
Frequently Asked Questions

Starting hormone replacement therapy after 50 raises specific questions about benefits, risks, and treatment options. Many women wonder about safety concerns, long-term effects, and how HRT compares to other menopause treatments.
What are the potential benefits of starting HRT after the age of 50?
HRT can provide significant relief from menopause symptoms even when started after 50. Hot flashes, night sweats, and sleep disruptions often improve within weeks of beginning treatment.
Bone health receives major protection from HRT. Estrogen helps maintain bone density and reduces the risk of osteoporosis-related fractures.
Many women experience better mood stability and mental clarity. Brain fog and memory issues that come with menopause may improve with hormone therapy.
Sexual health benefits include reduced vaginal dryness and improved libido. These changes can enhance quality of life and intimate relationships.
Heart health may benefit when HRT is started within 10 years of menopause[1] or before age 60. This timing is known as the “timing hypothesis.”
How might HRT affect your overall health if you begin treatment post-50?
Energy levels often increase as hormones stabilize. Many women report feeling more like their pre-menopause selves after starting treatment.
Sleep quality typically improves with HRT. Less frequent night sweats and better hormone balance contribute to more restful nights.
Skin and hair may show positive changes. Some women notice improved skin elasticity and reduced hair thinning.
Weight management can become easier. Hormones play a role in metabolism and fat distribution patterns.
Joint aches and stiffness may decrease. Estrogen has anti-inflammatory properties that can help with muscle and joint comfort.
What are the common indications that hormone replacement therapy is needed in individuals over 50?
Severe hot flashes that disrupt daily activities are a primary indicator. These episodes can interfere with work, sleep, and social situations.
Significant sleep disturbances from night sweats warrant consideration. Poor sleep affects overall health and quality of life.
Vaginal dryness and painful intercourse indicate declining estrogen levels. This condition, called genitourinary syndrome of menopause, responds well to hormone therapy.
Mood changes including anxiety, irritability, or depression may signal hormone imbalance. These symptoms often improve with HRT treatment.
Bone density loss detected on DEXA scans indicates increased fracture risk. HRT can help protect bone health in postmenopausal women.
Can you elaborate on the disadvantages or concerns associated with hormone replacement therapy for those over 50?
Breast cancer risk may increase slightly with certain types of HRT. The risk varies based on hormone types, delivery methods, and individual factors.
Blood clot risk can be higher with oral estrogen. Transdermal estrogen patches or gels carry lower clot risk[1] than pills.
Stroke risk may increase in some women. Age, smoking status, and cardiovascular health affect individual risk levels.
Gallbladder disease occurs more frequently with oral hormone therapy. Transdermal options may reduce this risk.
Side effects like breast tenderness, headaches, or mood changes can occur. These often improve as the body adjusts to treatment.
What should one be aware of regarding the long-term risks and safety of hormone replacement therapy after 50?
The five-year limit on HRT use came from outdated research, not medical necessity. Many people can take HRT for as long as they need to manage symptoms[14].
Individual risk assessment is crucial for long-term use. Personal and family medical history, lifestyle factors, and symptom severity all matter.
Regular monitoring with healthcare providers ensures safe continued use. Annual check-ups should include breast exams, blood pressure checks, and symptom assessment.
Bioidentical hormones may offer safety advantages over synthetic versions. These hormones are chemically identical to what the body naturally produces.
The 2002 Women’s Health Initiative study created unnecessary fear. Most participants were over 60 and used synthetic hormones, not bioidentical ones.
How does HRT compare to other treatments for age-related hormonal changes in people over 50?
Non-hormonal medications can help with hot flashes but don’t address other menopause symptoms. These include certain antidepressants and blood pressure medications.
Lifestyle changes like diet and exercise provide some benefit but may not be sufficient alone. They work well as complementary approaches to HRT.
Herbal supplements have limited scientific evidence for effectiveness. Black cohosh and soy isoflavones show mixed results in research studies.
Vaginal estrogen treats local symptoms without systemic hormone exposure. This option works well for women who only have vaginal dryness.
HRT provides the most comprehensive symptom relief for multiple menopause-related issues. It addresses hot flashes, sleep problems, mood changes, and bone health simultaneously.
References
- Is Hormone Replacement Therapy Safe After 50? What You Need to Know — Dr. Renee Wellenstein. https://www.drreneewellenstein.com/blog/is-hormone-replacement-therapy-safe-after-50-what-you-need-to-know Accessed November 8, 2025
- Menopause: Should You Quit HRT?. https://www.webmd.com/menopause/features/quitting-hormone-replacement-therapy Accessed November 8, 2025
- What happens to your body on HRT?. https://hormone-replacement-therapy.org/what-happens-to-your-body-on-hrt Accessed November 8, 2025
- Maintained muscle strength. https://www.nhs.gov.uk/medicines/hormone-replacement-therapy-hrt/benefits-and-risks-of-hormone-replacement-therapy-hrt/ Accessed November 8, 2025
- Menopause hormone therapy: Is it right for you?. https://www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/ART-20046372 Accessed November 8, 2025
- Benefits and risks of hormone replacement therapy (HRT). https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/benefits-and-risks-of-hormone-replacement-therapy-hrt/ Accessed November 8, 2025
- 403 Forbidden. https://www.cedars-sinai.org/blog/hormone-replacement-therapy-risks-benefits.html Accessed November 8, 2025
- Menopause hormone therapy: Is it right for you?. https://www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/art-20046372 Accessed November 8, 2025
- Types of hormone replacement therapy (HRT). https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/types-of-hormone-replacement-therapy-hrt/ Accessed November 8, 2025
- Research Studies on The Psychological Effects of HRT. https://www.pharmacyplanet.com/blog/post/research-studies-on-the-psychological-effects-of-hrt Accessed November 8, 2025
- Effects of Hormone Therapy on Cognition and Mood. https://pmc.ncbi.nlm.nih.gov/articles/PMC4330961/ Accessed November 8, 2025
- Taking a Closer Look at Menopausal Hormone Therapy and Cognitive Health. https://newsnetwork.mayoclinic.org/discussion/taking-a-closer-look-at-menopausal-hormone-therapy-and-cognitive-health/ Accessed November 8, 2025
- Hormone Replacement Therapy (HRT) for Menopause. https://my.clevelandclinic.org/health/treatments/15245-hormone-therapy-for-menopause-symptoms Accessed November 8, 2025
- Can you take HRT for the rest of your life? Benefits and risks. https://www.medicalnewstoday.com/articles/can-you-take-hrt-for-the-rest-of-your-life Accessed November 8, 2025
