Fifty years ago, meditation was dismissed as fringe, but today millions of Americans turn to mind-body practices for better health. Mind-body medicine includes practices like meditation, yoga, and mindfulness[1] that help reduce stress and improve both physical and mental well-being through the connection between thoughts, emotions, and bodily functions. Research now shows these techniques can lower blood pressure, reduce chronic pain, and help manage conditions from anxiety to heart disease.

The science behind mind-body medicine reveals how practices like meditation and breathing techniques[2] trigger measurable changes in the brain and body. These changes include reduced inflammation, improved heart rate patterns, and activation of the body’s natural relaxation response. What makes these approaches particularly appealing is that they work regardless of a person’s beliefs about them.
Healthcare systems are starting to recognize the value of these evidence-based practices. Medical schools now offer mind-body medicine courses[3], and doctors increasingly refer patients to stress management programs that teach these skills. As healthcare costs rise and stress-related diseases become more common, mind-body medicine offers a safe and effective way to complement traditional medical treatments.
Key Takeaways
- Mind-body medicine uses scientifically proven techniques like meditation and yoga to improve health through the mind-body connection
- These practices trigger measurable biological changes that reduce stress, lower blood pressure, and help manage chronic conditions
- Healthcare providers are increasingly integrating these evidence-based approaches into patient care as safe complements to traditional treatments
What Is Mind-Body Medicine?

Mind-body medicine represents a healthcare approach that recognizes the powerful connections between mental, emotional, and physical health. This field combines scientific understanding with practical techniques to help people manage stress, chronic pain, and various health conditions through the integration of mind and body healing practices.
Definition and Core Concepts
Mind-body medicine focuses on the interactions among the brain, mind, body, and behavior[4] to promote healing and wellness. This approach sees thoughts and emotions as having a direct impact on physical health.
The core concept involves the relaxation response. This is the opposite of the stress response that occurs during fight-or-flight situations. When people practice mind-body techniques, their bodies show measurable changes.
These changes include:
- Lower blood pressure
- Reduced heart rate
- Decreased oxygen use
- Less stress hormone production
Mind-body medicine includes various practices such as meditation, breathing techniques, tai chi, and yoga[2]. Each technique works to strengthen the connection between mental and physical states.
Psychoneuroimmunology forms the scientific foundation. This field studies how the nervous system, immune system, and hormones communicate with each other.
Historical Foundations and Evolution
Mind-body practices have roots in ancient traditions from many cultures. All major religions and cultures developed some form of meditation or contemplative practice throughout history.
Modern scientific study began about 50 years ago. Researchers first thought meditation was unusual and had no place in medical treatment. Early studies showed that meditation created measurable body changes.
The term “relaxation response” was coined to describe the coordinated set of physical changes that occur during mind-body practices. This research happened in the same lab where Walter Cannon had studied the stress response 50 years earlier.
Today, 14% of U.S. adults report using meditation and other mind-body practices within the previous year[1]. The current growth has happened mainly in secular settings rather than religious ones.
Medical schools now offer mind-body medicine classes. Some schools require these courses as part of their curriculum.
Differences From Conventional Medicine
Conventional medicine typically focuses on treating disease after it develops. Mind-body medicine works as both treatment and prevention by addressing the root causes of stress-related illness.
Studies show that 60 to 80% of primary care visits have a stress-related component[1]. Traditional medicine often uses medications and procedures to treat symptoms.
Key Differences:
| Conventional Medicine | Mind-Body Medicine |
|---|---|
| Disease treatment model | Health enhancement model |
| External interventions | Self-care techniques |
| Symptom focused | Whole-person approach |
| Reactive care | Preventive care |
Mind-body medicine works as CAM (complementary and alternative medicine). It can be used alongside conventional treatments to improve outcomes.
The approach helps people develop coping skills and resilience. Patients learn techniques they can use on their own to manage stress and symptoms.
Research shows improved outcomes for chronic pain, anxiety, depression, and cardiovascular disease[1] when mind-body techniques are added to regular treatment. Insurance coverage remains limited, so many people pay out of pocket for these services.
How Mind-Body Medicine Works

Mind-body medicine works through interactions between the brain, mind, body, and behavior[2] to affect how the body functions. The brain sends signals through the nervous system that control stress hormones like cortisol and activate either fight-or-flight responses or calming relaxation states.
Brain-Body Communication Pathways
The brain communicates with the body through complex networks of nerves, hormones, and chemical messengers. These pathways carry information in both directions between the brain and organs.
Neural pathways connect the brain to every part of the body through the spinal cord and peripheral nerves. The brain processes thoughts, emotions, and sensations, then sends signals that affect heart rate, breathing, and muscle tension.
Hormonal communication happens when the brain releases chemicals into the bloodstream. The hypothalamus in the brain controls hormone release from glands throughout the body. These hormones influence mood, energy levels, and immune function.
Chemical messengers called neurotransmitters carry signals between brain cells. Dopamine, serotonin, and other neurotransmitters affect how a person feels and how their body responds to stress or relaxation.
The brain also receives feedback from the body about pain, temperature, and other sensations. This two-way communication allows mental states to influence physical health and physical changes to affect mental well-being.
Stress Response and Relaxation Response
The stress response activates when the brain perceives danger or pressure. The sympathetic nervous system triggers the release of stress hormones like cortisol and adrenaline.
Fight-or-flight activation happens quickly during stressful situations. Heart rate increases, breathing becomes faster, and muscles tense up. Blood flow shifts to major muscle groups to prepare for action.
Cortisol levels rise during chronic stress, which can weaken the immune system and cause health problems over time. High cortisol affects sleep, digestion, and blood sugar levels.
The relaxation response works as the opposite of the stress response. Mind-body techniques can activate this calming state[5] through meditation, deep breathing, or other practices.
During relaxation, heart rate slows down, blood pressure drops, and muscle tension decreases. The body releases fewer stress hormones and more calming chemicals. This state helps the body heal and restore itself.
Role of the Nervous System
The nervous system controls how mind-body medicine affects the body. It has two main parts that work together to manage stress and relaxation responses.
The sympathetic nervous system activates during stress and emergency situations. It speeds up the heart, increases breathing rate, and releases stress hormones. This system helps people respond quickly to threats.
The parasympathetic nervous system promotes rest and recovery. It slows the heart rate, improves digestion, and helps the body conserve energy. This system becomes more active during relaxation and sleep.
Mind-body practices can train people to activate the parasympathetic nervous system more easily. Techniques like meditation and deep breathing send signals through the nervous system that promote calm states.
The nervous system also processes pain signals and emotional responses. Mind-body interventions can change how these signals are interpreted[6], potentially reducing pain and improving mood.
Regular practice helps strengthen the pathways that promote relaxation and stress management. The nervous system becomes better at switching between active and calm states as needed.
Key Mind-Body Medicine Therapies and Techniques
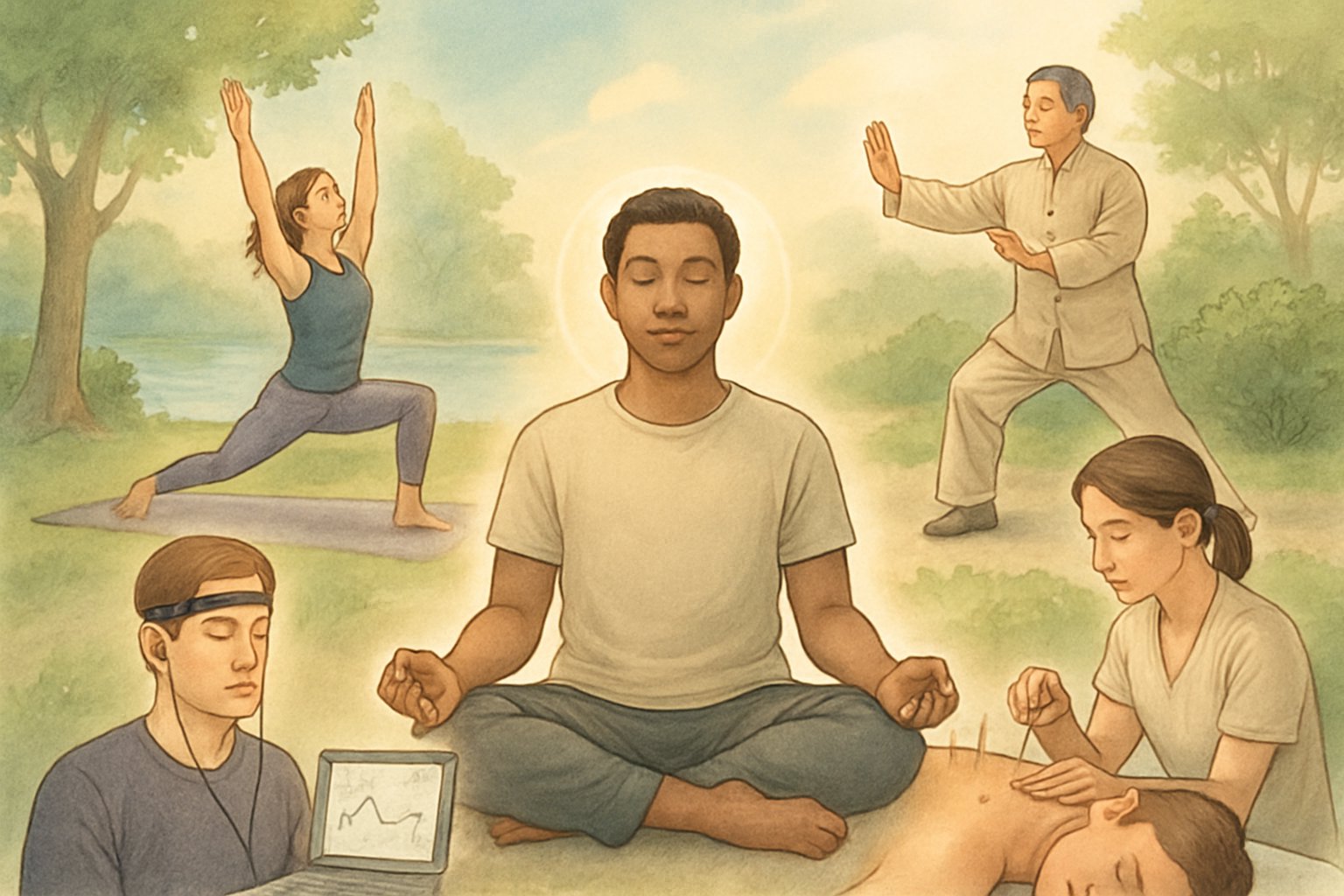
Several proven mind-body therapies[6] help people manage stress, reduce pain, and improve their overall health. These healing techniques[7] work by strengthening the connection between mental and physical well-being.
Meditation and Mindfulness
Meditation involves focusing the mind on a single point of attention to achieve mental clarity and emotional calm. Meditation practices[8] can include concentrating on breathing, repeating mantras, or observing thoughts without judgment.
Regular meditation strengthens the brain’s prefrontal cortex. This area controls decision-making and emotional regulation.
Mindfulness meditation teaches people to stay present in the moment. Practitioners learn to notice their thoughts, feelings, and body sensations without trying to change them.
Common meditation types include:
- Focused attention meditation – concentrating on breath or a specific object
- Open monitoring meditation – observing all thoughts and sensations
- Loving-kindness meditation – sending positive thoughts to others
Research shows that consistent meditation practice can lower blood pressure and reduce anxiety. Many people report better sleep quality and improved focus after regular sessions.
Yoga and Movement Practices
Yoga combines physical poses, breathing exercises, and meditation[2] to promote both physical and mental health. The practice originated in ancient India and includes many different styles and approaches.
Physical yoga poses, called asanas, help improve flexibility, strength, and balance. The breathing component, known as pranayama, teaches controlled breathing patterns that calm the nervous system.
Popular yoga styles include:
- Hatha yoga – gentle poses held for several breaths
- Vinyasa yoga – flowing movements linked with breath
- Restorative yoga – relaxing poses using props for support
Tai chi[8] is another movement practice that combines slow, flowing motions with deep breathing and meditation. This gentle exercise improves balance and reduces stress.
Both yoga and tai chi can help reduce chronic pain and improve mood. These practices work well for people of all ages and fitness levels.
Biofeedback and Deep Breathing
Biofeedback uses electronic devices to help people learn to control body functions[9] they normally cannot feel or control. Sensors attached to the body measure things like heart rate, muscle tension, or brain waves.
The devices provide real-time feedback through sounds or visual displays. This information helps people recognize when their body is stressed and learn techniques to relax.
Common biofeedback types monitor:
- Heart rate variability
- Muscle tension levels
- Skin temperature changes
- Brain wave patterns
Deep breathing exercises form a key part of many mind-body interventions[10]. Controlled breathing activates the body’s relaxation response and reduces stress hormones.
Diaphragmatic breathing involves breathing deeply into the belly rather than the chest. This technique slows the heart rate and lowers blood pressure naturally.
Guided Imagery and Hypnosis
Guided imagery uses the power of imagination to promote healing and relaxation. Practitioners visualize peaceful scenes or positive outcomes while in a relaxed state.
Mental healing through imagery[9] can help manage pain, reduce anxiety, and improve immune function. Many people use recorded audio guides or work with trained therapists.
The technique works by engaging multiple senses in the imagination. People might picture healing light flowing through their body or visualize themselves in a calm natural setting.
Hypnosis involves entering a focused, trance-like state[9] where the mind becomes more open to positive suggestions. Clinical hypnosis differs from stage hypnosis and always keeps the person in control.
Medical hypnosis can help with pain management, habit changes, and stress reduction. Trained therapists guide patients into relaxed states where healing suggestions become more effective.
Both techniques tap into the mind’s natural ability to influence physical health through focused mental activity.
Health Benefits and Clinical Applications

Mind-body medicine provides measurable benefits for stress reduction, mental health conditions, and pain management. Research shows these practices can lower anxiety and depression symptoms while helping people develop better coping skills for chronic conditions.
Stress Relief and Well-Being
Mind-body practices reduce stress[1] by activating the relaxation response, which lowers blood pressure and heart rate. This creates physical changes that are opposite to the fight-or-flight response.
Regular meditation and yoga help people feel less stressed in daily life. Studies show these techniques improve heart rate variability and reduce stress hormones in the body.
The relaxation response happens during many mind-body practices. It helps the nervous system calm down and promotes better sleep patterns.
Key stress-relief benefits include:
- Lower blood pressure and heart rate
- Reduced stress hormone levels
- Better sleep quality
- Increased sense of well-being
Many people notice they feel more relaxed after just a few weeks of practice. The benefits often continue to grow with regular use over time.
Mental Health: Anxiety, Depression, and Coping Skills
Mind-body techniques significantly reduce symptoms of anxiety and depression[11]. These practices teach people new ways to handle difficult emotions and stressful situations.
Meditation helps people observe their thoughts without getting caught up in them. This skill is especially helpful for managing anxiety and worry patterns.
Mental health improvements include:
- Reduced anxiety symptoms
- Less severe depression
- Better emotional control
- Improved coping strategies
These techniques work well alongside traditional therapy and medication. People learn to notice early warning signs of stress and respond in healthier ways.
Research shows that regular practice helps build resilience over time. People become better at bouncing back from difficult life events and daily challenges.
Chronic Pain and Headache Management
Mind-body medicine helps manage chronic pain[12] by changing how the brain processes pain signals. These techniques are particularly useful for headaches and migraines.
Relaxation practices reduce muscle tension that often makes pain worse. They also help people cope better with ongoing pain conditions.
Pain management benefits:
- Reduced pain intensity
- Less frequent headaches
- Better pain coping skills
- Decreased need for pain medications
Many people with chronic pain find they can do more daily activities after learning these techniques. The practices help break the cycle of pain, stress, and muscle tension.
Guided imagery and meditation teach the mind to focus away from pain. This doesn’t eliminate pain completely but makes it more manageable for most people.
Physical Health Impacts and Disease Management

Mind-body medicine demonstrates measurable effects on chronic diseases including cardiovascular conditions, diabetes, and cancer[13]. These interventions work through complex biological pathways that regulate inflammation, stress hormones, and immune system function.
Cardiovascular Health and Hypertension
Mind-body practices directly influence cardiovascular disease through multiple mechanisms. Meditation and relaxation techniques activate the parasympathetic nervous system, which lowers heart rate and reduces blood pressure.
Research shows that regular meditation can decrease systolic blood pressure by 3-5 mmHg in patients with hypertension. This reduction is clinically significant and comparable to some medications.
Key cardiovascular benefits include:
- Reduced resting heart rate
- Improved heart rate variability
- Lower inflammatory markers
- Decreased cortisol levels
Breathing exercises specifically target the autonomic nervous system. Deep breathing patterns slow heart rate and promote vasodilation, leading to immediate blood pressure reductions.
Yoga combines physical movement with mindfulness, offering dual benefits for cardiovascular health. Studies demonstrate that regular yoga practice can reduce cardiovascular disease risk factors by improving circulation and reducing arterial stiffness.
Primary care physicians increasingly recommend these techniques as adjunct treatments for hypertension management. Patients often see improvements within 8-12 weeks of consistent practice.
Diabetes and Obesity
Mind-body interventions show promise in diabetes management through stress reduction and behavioral modification. Chronic stress elevates cortisol levels, which directly impacts blood sugar regulation and insulin sensitivity.
Meditation practices help patients develop better awareness of hunger cues and emotional eating patterns. This awareness is crucial for sustainable weight management in obesity treatment.
Diabetes-specific benefits include:
- Improved glucose tolerance
- Better medication adherence
- Reduced diabetic complications
- Enhanced self-care behaviors
Mindfulness-based interventions teach patients to recognize stress-induced eating triggers. This skill is particularly valuable for individuals with type 2 diabetes who struggle with weight management.
Studies indicate that patients practicing regular meditation show improved HbA1c levels over 6-month periods. The improvements stem from both direct physiological effects and enhanced self-management behaviors.
Tai chi and qigong offer gentle exercise options for diabetic patients with mobility limitations. These practices improve balance, reduce fall risk, and provide moderate cardiovascular benefits without joint stress.
Cancer Care and Autoimmune Conditions
Cancer patients using mind-body techniques report reduced treatment-related side effects and improved quality of life. These practices don’t cure cancer but significantly impact the treatment experience.
Meditation and guided imagery help manage chemotherapy-induced nausea and treatment anxiety. Patients often require fewer anti-nausea medications when combining conventional treatments with these approaches.
Immune system benefits include:
- Reduced systemic inflammation
- Improved natural killer cell activity
- Better treatment tolerance
- Enhanced emotional resilience
Patients with rheumatoid arthritis (RA) experience decreased joint pain and stiffness through regular meditation practice. The anti-inflammatory effects help reduce disease activity markers.
Mindfulness-based stress reduction programs show particular effectiveness in autoimmune conditions. The practice helps regulate the overactive immune responses characteristic of these diseases.
Cancer support groups incorporating mind-body techniques demonstrate improved survival rates in some studies. The combination of social support and stress reduction creates synergistic healing effects.
Insomnia and Sleep Disorders
Sleep disorders respond well to mind-body interventions, often providing alternatives to sleep medications. These techniques address both the physical and mental factors contributing to insomnia.
Progressive muscle relaxation helps patients release physical tension that interferes with sleep onset. The systematic tensing and releasing of muscle groups promotes natural relaxation responses.
Sleep improvement mechanisms:
- Reduced cortisol at bedtime
- Quieted mental chatter
- Improved sleep hygiene awareness
- Enhanced circadian rhythm regulation
Meditation before bedtime activates the parasympathetic nervous system, preparing the body for restorative sleep. Regular practitioners report falling asleep faster and experiencing deeper sleep cycles.
Cognitive techniques help patients break the anxiety-insomnia cycle that perpetuates sleep problems. Learning to observe racing thoughts without engagement reduces bedtime mental activation.
Sleep-focused mindfulness programs show success rates comparable to cognitive behavioral therapy for insomnia. Patients typically see improvements within 4-6 weeks of consistent practice.
Integrating Mind-Body Medicine Into Healthcare

Healthcare systems are adopting mind-body medicine through structured frameworks that address primary care needs, safety considerations, and implementation strategies. The BERN framework integrates behavioral modification, exercise, relaxation, and nutrition[14] into comprehensive treatment approaches.
Role in Primary and Preventive Care
Primary care providers increasingly use mind-body medicine for lifestyle-related chronic diseases. MBM addresses musculoskeletal complaints, metabolic disorders, high blood pressure, and gastrointestinal dysfunction[14] commonly seen in general practice.
The two-door model separates traditional medical treatment from mind-body interventions. Physicians handle diagnosis and pathology treatment while trained coaches implement behavioral and lifestyle modifications.
Primary applications include:
- Type 2 diabetes management
- Chronic pain disorders
- Stress-related conditions
- Cancer treatment support
- Addiction recovery assistance
Healthcare providers enhance patient care by integrating meditation practices into clinical work[10]. This approach focuses on health promotion rather than disease treatment alone.
Preliminary findings suggest these integrative tools may reduce healthcare utilization and prove cost-effective[1]. The preventive focus helps patients develop self-regulation skills.
Considerations and Contraindications
Mind-body medicine presents low risk for most patients when properly implemented. Healthcare providers must assess individual readiness and capacity for behavioral change programs.
Key considerations include:
- Patient motivation levels
- Cognitive capacity for self-regulation
- Physical limitations affecting exercise components
- Mental health stability for relaxation practices
Contraindications are minimal but exist for specific healing techniques. Intensive meditation may not suit patients with certain psychiatric conditions. Physical exercise components require modification for mobility limitations.
Training barriers exist for healthcare providers seeking to integrate MBM into primary care[15]. Systematic changes in medical education and practice structures are needed.
Risk assessment focuses on implementation quality rather than technique dangers. Improperly trained instructors may reduce effectiveness rather than cause harm.
Perspectives on Future Directions
Healthcare integration continues expanding through institutional support and research validation. Medical education programs now include mind-body approaches like meditation, guided imagery, and biofeedback[16].
Emerging trends include:
- Technology-assisted delivery methods
- Personalized intervention protocols
- Integration with conventional treatments
- Expanded insurance coverage
Organizations like the Benson-Henry Institute work to integrate mind-body medicine into mainstream healthcare[17] nationally and globally. This institutional backing accelerates adoption.
Future directions emphasize evidence-based protocols and standardized training. Healthcare systems require consistent implementation methods to ensure quality outcomes.
Research focuses on identifying which patients benefit most from specific MBS interventions. Personalized medicine approaches may optimize treatment selection and improve cost-effectiveness ratios.
Frequently Asked Questions

Mind-body medicine combines scientific evidence with practical approaches to healing that address both mental and physical well-being. Common questions focus on specific therapeutic techniques, health outcomes, professional training requirements, and how these practices integrate with traditional medical care.
What are the primary therapies associated with mind-body medicine?
Mind-body medicine involves intentional movement and breathing techniques[18] as core therapeutic approaches. Meditation, journaling, and mindfulness practices form the foundation of most treatment programs.
Hypnosis represents another established therapy within this field. Practitioners often address questions about hypnosis safety and effectiveness[19] with patients considering this treatment option.
Group therapy sessions provide structured environments for learning mind-body skills. Many programs combine individual practice with group support to enhance therapeutic outcomes.
How does mind-body medicine impact physical health?
Mind-body medicine focuses on interactions between mind and body, showing how emotional, mental, social and spiritual factors directly relieve stress[5] and improve overall health. Research demonstrates measurable improvements in pain management, immune function, and cardiovascular health.
Stress reduction serves as a primary pathway for physical health benefits. Lower stress hormones lead to decreased inflammation and improved healing responses throughout the body.
Patients often experience better sleep quality, reduced chronic pain, and improved digestive function. These physical improvements typically develop alongside enhanced emotional well-being and mental clarity.
What educational paths are available for a career in mind-body medicine?
Healthcare professionals can pursue specialized training through accredited mind-body medicine programs. Medical doctors, nurses, therapists, and counselors often complete additional coursework to integrate these approaches into their practice.
Certificate programs offer structured pathways for learning evidence-based mind-body techniques. These programs typically include both theoretical foundations and hands-on skill development.
Some practitioners combine mind-body training with existing specialties like physical medicine, sports medicine, or neurology. This integration allows professionals to offer comprehensive treatment approaches within their established practice areas.
What are the benefits of obtaining a mind-body medicine certification?
Certification in mind-body medicine provides professional recognition and validates expertise[20] in evidence-based therapeutic approaches. Certified practitioners gain access to specialized treatment protocols and continuing education resources.
Professional certification enhances credibility with patients and healthcare colleagues. Many healthcare systems now recognize and seek providers with mind-body medicine credentials.
Certified practitioners often report increased job satisfaction and expanded treatment options for their patients. The certification process also provides networking opportunities with other mind-body medicine professionals.
How is mind-body medicine integrated into conventional healthcare practices?
Military medical centers like Walter Reed incorporate mind-body medicine into comprehensive pain management programs[21]. These programs demonstrate successful integration within traditional medical settings.
Healthcare systems often begin integration by offering group classes and workshops. Programs typically run multiple sessions per year with scheduled meeting times[22] to accommodate different patient schedules.
Practitioners frequently work alongside conventional medical teams to provide complementary care. This collaborative approach ensures patients receive both traditional medical treatment and mind-body interventions as appropriate.
What research supports the efficacy of mind-body medicine?
Mind-body skills are scientifically validated to reduce stress and restore physical and psychological health[5]. Multiple clinical trials demonstrate effectiveness for conditions including chronic pain, anxiety, and depression.
Neuroimaging studies show measurable brain changes following mind-body interventions. These studies reveal improved emotional regulation and stress response patterns in participants.
Research consistently shows positive outcomes for both individual therapy and group-based programs. Studies demonstrate benefits across diverse populations and various medical conditions, supporting widespread clinical application.
References
- A New Era for Mind–Body Medicine. https://pmc.ncbi.nlm.nih.gov/articles/PMC7486127/ Accessed November 13, 2025
- What is Mind-Body Medicine?. https://health.ucdavis.edu/integrative-medicine/clinical-care/mind-body-medicine.html Accessed November 13, 2025
- Harvard CME. https://mindbody.hmscme.com/ Accessed November 13, 2025
- Mind-body medicine focuses on the interactions among the brain, mind, body, and behavior. https://sandiego.tricare.mil/Portals/124/What%20is%20Mind%20Body%20Medicine.pdf Accessed November 13, 2025
- What is mind-body medicine?. https://cmbm.org/faq/what-is-mind-body-medicine/ Accessed November 13, 2025
- Integrative Medicine: About Mind-Body Therapies. https://www.mskcc.org/cancer-care/diagnosis-treatment/symptom-management/integrative-medicine/mind-body Accessed November 13, 2025
- ScienceDirect. https://www.sciencedirect.com/topics/medicine-and-dentistry/mind-body-medicine Accessed November 13, 2025
- Mind and Body Practices. https://www.nccih.nih.gov/health/mind-and-body-practices Accessed November 13, 2025
- Mind-Body Therapies - MeSH. https://www.ncbi.nlm.nih.gov/mesh/?term=%22mind-body%20therapies%22%5BMeSH%20Terms%5D%20OR%20Mind-Body%20Therapies%5BText%20Word%5D&cmd=DetailsSearch Accessed November 13, 2025
- Exploring Mind-Body Medicine For Better Health – UC Davis Health Office of Wellness Education. https://wellness.ucdavis.edu/videos/exploring-mind-body-medicine-for-better-health/ Accessed November 13, 2025
- The Power of Mind-Body Medicine. https://www.westeasternhealth.com/the-power-of-mind-body-medicine/ Accessed November 13, 2025
- 7 Benefits of Mind-Body Medicine for Trauma Survivors. https://casatondemand.org/2023/02/07/7-benefits-of-mind-body-medicine-for-trauma-survivors/ Accessed November 13, 2025
- Frontiers. https://www.frontiersin.org/journals/integrative-neuroscience/articles/10.3389/fnint.2023.1188638/full Accessed November 13, 2025
- The BERN Framework of Mind-Body Medicine: Integrating Self-Care, Health Promotion, Resilience, and Applied Neuroscience. https://pmc.ncbi.nlm.nih.gov/articles/PMC9330052/ Accessed November 13, 2025
- Training barriers exist for healthcare providers seeking to integrate MBM into primary care. https://www.bu.edu/familymed/files/2016/08/Journal.pdf Accessed November 13, 2025
- Mind Body Medicine Program | Medical Education | Georgetown University. https://meded.georgetown.edu/medicaleducation/mindbody/ Accessed November 13, 2025
- Benson-Henry Institute for Mind Body Medicine. https://www.massgeneral.org/psychiatry/treatments-and-services/benson-henry-institute Accessed November 13, 2025
- Mind-Body Medicine. https://www.texascenterforlifestylemedicine.org/mind-body-medicine Accessed November 13, 2025
- Just a moment.... https://mindbodymedicine.artsandsciences.baylor.edu/about/frequently-asked-questions Accessed November 13, 2025
- Certification: Frequently Asked Questions. https://cmbm.org/certification-frequently-asked-questions/ Accessed November 13, 2025
- Mind Body Medicine. https://walterreed.tricare.mil/About-Us/Wounded-Warrior-Care/Wounded-Warrior-Pain-Care-Initiative/Mind-Body-Medicine Accessed November 13, 2025
- Department of Neurological Sciences. https://www.med.uvm.edu/mbmc/clinical_faq Accessed November 13, 2025
