Your kidneys work around the clock to filter waste and extra water from your blood. When these vital organs begin to fail, your body struggles to remove toxins and maintain proper fluid balance. Kidney failure occurs when your kidneys lose 85-90% of their function, meaning they can no longer filter waste effectively enough to keep you healthy.
The process usually happens slowly over months or years. Diabetes and high blood pressure are the most common causes[1] of kidney failure, though the condition can also develop suddenly due to injury or illness. Many people don’t notice symptoms in the early stages, which makes kidney disease particularly dangerous.
As kidney function declines, waste products build up in your blood and cause serious health problems. Your body may retain too much fluid, leading to swelling and breathing difficulties. Without treatment like dialysis or a kidney transplant, end-stage kidney failure can be life-threatening[1].
Key Takeaways
- Kidney failure happens when your kidneys lose most of their ability to filter waste from your blood
- Early kidney disease often has no symptoms, making regular checkups important for people at risk
- Treatment options like dialysis and transplants can help people live with kidney failure, but there is no cure
Understanding Kidney Function and the Role of the Kidneys
The kidneys are vital organs that filter waste from blood, regulate blood pressure, and maintain the body’s chemical balance. Each kidney contains millions of tiny filters that work together to keep the body healthy and remove harmful substances.
How Healthy Kidneys Work
Most people have two kidneys located on either side of the spine below the rib cage. Each kidney is about the size of an adult fist[2] and contains up to one million tiny filtering units called nephrons.
The kidneys follow a specific filtering process every day. Blood enters the kidneys through an artery from the heart[2] and passes through millions of tiny blood filters. These filters separate waste materials from useful substances in the blood.
Clean blood returns to the body through veins. Waste materials travel through tubes called ureters to the bladder as urine. The kidneys filter about 200 quarts of fluid from blood each day[2].
Most filtered fluid gets cleaned and returned to the body. Only about 2 quarts become urine that leaves the body.
Kidney Function in the Body
The kidneys perform many important jobs beyond filtering blood. They help remove waste and excess fluid from the body[2] while keeping necessary substances.
Key kidney functions include:
- Filtering blood and removing toxins
- Making red blood cells[2]
- Balancing important vitamins and minerals[2]
- Maintaining blood pressure[2]
- Keeping bones healthy[2]
The kidneys also control the body’s fluid balance. They decide how much water to keep and how much to remove as urine. This process helps maintain proper blood pressure and prevents swelling.
Healthy kidney function depends on good blood flow. If blood flow gets blocked, parts of the kidney can die and lead to kidney failure.
Importance of Glomerular Filtration Rate (GFR)
Glomerular filtration rate measures how well the kidneys filter blood. GFR shows how much blood passes through the kidney filters each minute. Doctors use this number to check kidney health.
The estimated glomerular filtration rate (eGFR) is a blood test that measures kidney function. This test measures creatinine, a waste product from muscle breakdown[2]. Higher creatinine levels mean lower kidney function.
Normal GFR ranges:
- 90 or above: Normal kidney function
- 60-89: Mild decrease in kidney function
- 30-59: Moderate decrease in kidney function
- 15-29: Severe decrease in kidney function
- Below 15: Kidney failure
Regular testing can find kidney problems early[2]. Early detection helps doctors start treatment before kidney damage gets worse. Many people with kidney disease have no symptoms until the condition becomes serious.
What Kidney Failure Means
Kidney failure occurs when the kidneys lose their ability to filter waste and excess fluid from the blood effectively. This condition can develop gradually over years or happen suddenly within hours or days, requiring immediate medical attention to prevent life-threatening complications.
Definition of Kidney Failure
Kidney failure is a condition in which one or both kidneys no longer work on their own[1]. Medical professionals also call this condition renal failure or end-stage renal disease.
The kidneys normally filter about 50 gallons of blood each day. They remove waste products, extra water, and toxins through urine.
When less than 15% of kidney function remains, doctors diagnose kidney failure[3]. At this stage, the kidneys cannot maintain the body’s chemical balance.
End-stage kidney disease (ESRD) represents the final stage of chronic kidney disease. People with ESRD need dialysis or a kidney transplant to survive.
Loss of Kidney Function
Kidney failure means 85-90% of normal kidney function is gone[4]. The remaining kidney tissue cannot handle the body’s needs.
Healthy kidneys perform several vital functions:
- Filter waste and toxins from blood
- Control fluid balance
- Regulate blood pressure
- Produce hormones for red blood cell production
- Balance important minerals like sodium and potassium
When kidneys fail, these functions stop working properly. Waste products build up in the blood and become toxic to other organs.
The body cannot maintain proper fluid balance. This leads to dangerous swelling and breathing problems.
Blood chemistry becomes unstable. Electrolyte imbalances can cause heart rhythm problems and muscle weakness.
Acute vs. Chronic Kidney Failure
Acute kidney failure develops suddenly, usually within hours or days. Medical professionals call this acute kidney injury (AKI).
Acute kidney failure may develop within hours or days and is often temporary[1]. Common causes include severe dehydration, certain medications, or blocked urine flow.
Many people recover full kidney function from acute kidney injury with proper treatment. Early medical care is critical for the best outcomes.
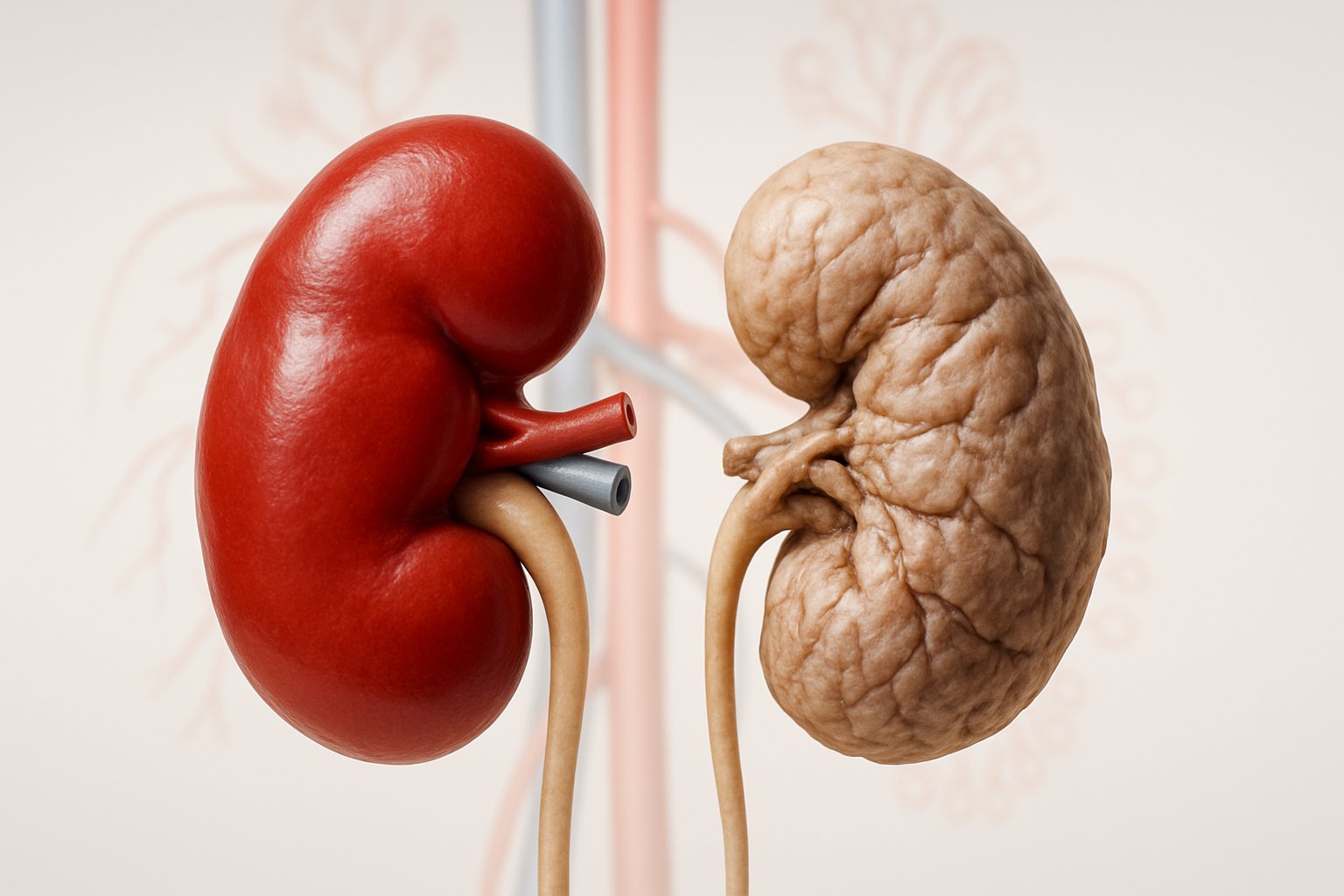
Chronic kidney failure develops slowly over months or years. This gradual decline often goes unnoticed in early stages.
Diabetes and high blood pressure are the most common causes of chronic kidney disease[1]. These conditions damage kidney tissue over time.
Chronic kidney failure is permanent. Treatment focuses on slowing progression and managing complications rather than curing the condition.
Stages and Progression of Kidney Disease

Kidney disease progresses through five distinct stages, with each stage showing increasing damage and declining function. The final stage requires dialysis or transplant, while earlier stages may slow progression through treatment.
Stages of Chronic Kidney Disease
Chronic kidney disease progresses through five stages[5] based on kidney function levels. Doctors measure this using a blood test called eGFR.
Stage 1 shows normal kidney function with mild damage. The eGFR remains above 90. Many people have no symptoms at this stage.
Stage 2 indicates mild decline with eGFR between 60-89. Kidney damage becomes more noticeable but symptoms stay minimal.
Stage 3 splits into two parts. Stage 3a has eGFR of 45-59, while stage 3b ranges from 30-44. People may start feeling tired and notice swelling.
Stage 4 represents severe decline with eGFR between 15-29. Symptoms become more obvious. Patients should prepare for kidney replacement therapy.
Stage 5 means kidney failure with eGFR below 15[4]. This stage requires immediate treatment to survive.
| Stage | eGFR Range | Kidney Function | Symptoms |
|---|---|---|---|
| 1 | 90+ | Normal with damage | Usually none |
| 2 | 60-89 | Mild decrease | Minimal |
| 3a | 45-59 | Moderate decrease | Fatigue, swelling |
| 3b | 30-44 | Moderate decrease | More noticeable |
| 4 | 15-29 | Severe decrease | Significant symptoms |
| 5 | <15 | Kidney failure | Life-threatening |
Transition to End-Stage Renal Disease
End-stage renal disease occurs when 85-90% of kidney function disappears[4]. This represents the final stage of chronic kidney disease progression.
The transition happens gradually over months or years. Kidneys lose their ability to filter waste and excess fluid from blood. Toxins build up in the body causing serious health problems.
Symptoms become severe during this transition. People experience extreme fatigue, nausea, and difficulty breathing. Swelling in legs and feet becomes pronounced.
Key signs of progression include:
- Urinating less frequently or not at all
- Severe muscle cramps and weakness
- Mental confusion and difficulty concentrating
- Loss of appetite and weight loss
Once patients reach this stage, they need dialysis or kidney transplant to survive. Without treatment, the condition becomes fatal within weeks or months.
Nephrotic Syndrome and Kidney Damage
Nephrotic syndrome represents a specific type of kidney damage that affects protein filtration. The kidneys leak large amounts of protein into urine instead of keeping it in blood.
This condition causes the body to lose essential proteins. Blood protein levels drop significantly while urine protein increases dramatically.
Primary symptoms include:
- Severe swelling in face, legs, and abdomen
- Foamy or frothy urine appearance
- Weight gain from fluid retention
- High cholesterol levels
Nephrotic syndrome can occur at any stage of kidney disease. It often indicates serious damage to the kidney’s filtering units called glomeruli.
The condition increases risk of infections and blood clots. Patients may develop complications like kidney failure if left untreated.
Treatment focuses on controlling protein loss and managing symptoms. Medications help reduce inflammation and protect remaining kidney function.
Signs and Symptoms of Kidney Failure
Kidney failure develops gradually, with symptoms often appearing only after significant damage has occurred. The most common early warning signs include extreme tiredness, swelling, and changes in urination[1], while advanced stages bring more severe complications affecting multiple body systems.
Early Signs of Declining Kidney Function
Many people experience few symptoms during the initial stages of kidney disease. The kidneys can lose up to 90% of their function before noticeable signs appear.
Fatigue ranks among the earliest indicators of kidney problems. Healthy kidneys produce a hormone called erythropoietin that signals the body to make red blood cells[6]. When kidney function declines, red blood cell production drops, leading to anemia and persistent tiredness.
Changes in urination patterns often occur early in the disease process. People may notice they urinate more frequently, especially at night, or produce less urine than usual.
Subtle swelling may develop around the eyes, hands, or feet. This happens because damaged kidneys cannot remove excess fluid effectively from the body.
Loss of appetite can begin during early stages. Food may taste different or have a metallic flavor as waste products build up in the bloodstream.
Advanced Symptoms of Kidney Failure
As kidney function deteriorates further, symptoms become more pronounced and affect daily activities[1].
Severe swelling (edema) becomes more noticeable, particularly around the ankles, hands, and face. Fluid retention can cause rapid weight gain and difficulty fitting into shoes or clothing.
Nausea and vomiting increase in frequency and intensity. The buildup of waste products in the blood creates toxins that affect the digestive system and overall well-being.
Muscle cramps develop as electrolyte imbalances worsen. The kidneys struggle to maintain proper levels of sodium, potassium, and other essential minerals in the blood.
Persistent itching occurs throughout the body as waste products accumulate under the skin. This symptom can be particularly bothersome and interfere with sleep.
Shortness of breath may develop due to fluid accumulation around the lungs or severe anemia reducing oxygen-carrying capacity.
Physical and Cognitive Changes
Advanced kidney failure affects both physical appearance and mental function as toxins accumulate throughout the body.
Cognitive symptoms include confusion, difficulty concentrating, and memory problems. These changes occur because waste products that should be filtered by healthy kidneys remain in the bloodstream and affect brain function.
Skin changes become more apparent, including dryness, unusual coloring, and persistent itching. Some people develop a condition where skin appears darker or yellowish due to waste buildup.
Sleep disturbances commonly occur due to physical discomfort, frequent urination, muscle cramps, and restless leg syndrome.
Severe fatigue intensifies as anemia worsens and the body struggles to maintain energy levels. Simple daily activities become increasingly difficult to complete.
Temperature regulation problems may cause unexplained fever or feeling constantly cold as the kidneys lose their ability to help regulate body temperature and fluid balance.
Common Complications of Kidney Failure
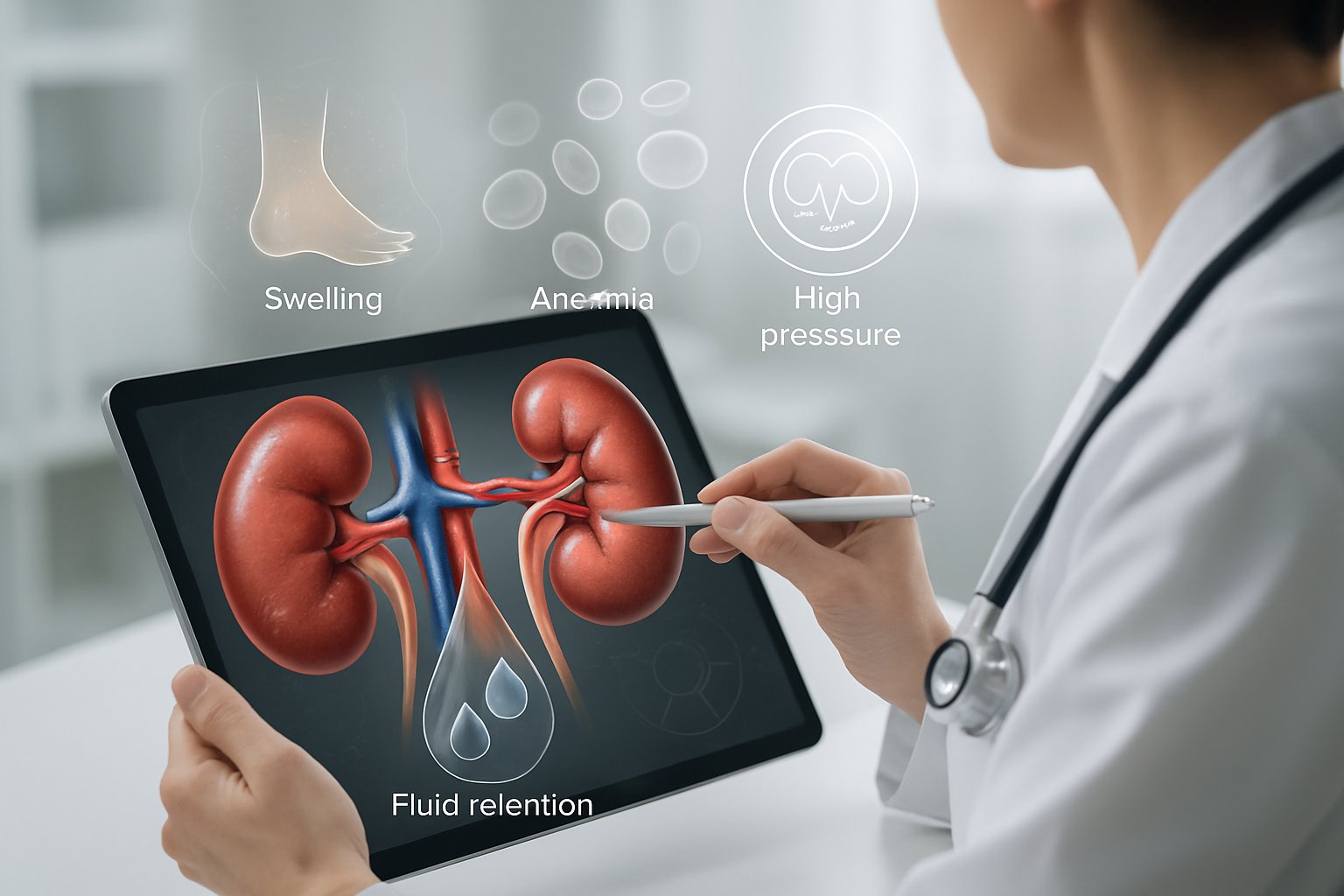
When kidneys fail, complications affect many body systems[7] because these organs control fluid balance, blood pressure, and waste removal. The body struggles with dangerous mineral imbalances, heart problems from fluid buildup, and toxic waste accumulation.
Fluid, Electrolyte, and Mineral Imbalances
Failed kidneys cannot properly balance fluids and minerals in the body. This leads to dangerous changes in blood chemistry.
Hyperkalemia occurs when potassium levels become too high. The heart muscle becomes affected, which can cause deadly heart rhythm problems. Patients must limit foods like bananas, potatoes, and oranges.
Calcium and phosphorus imbalances develop as kidney function declines. Phosphorus builds up in the blood while calcium levels drop. This creates mineral and bone disorder, making bones weak and brittle.
Metabolic acidosis happens when the kidneys cannot remove acid from the blood. The body becomes too acidic, which affects breathing and bone health. Patients may need special medications to control acid levels.
Fluid retention causes swelling in the legs, ankles, and around the eyes. Some people gain weight quickly from excess fluid buildup.
Heart, Blood, and Bone-Related Risks
Kidney failure puts severe stress on the heart and blood vessels. Heart disease becomes a major risk[8] for people with failed kidneys.
High blood pressure worsens as the kidneys cannot control fluid balance. Blood pressure often becomes hard to control even with multiple medications. This increases the risk of stroke and heart failure.
Anemia develops because kidneys make a hormone called erythropoietin that tells the body to produce red blood cells. Without this hormone, red blood cell counts drop dangerously low. Patients feel tired, weak, and short of breath.
The combination of fluid retention and anemia forces the heart to work much harder. This can lead to heart failure, where the heart cannot pump blood effectively throughout the body.
Uremia and Related Complications
Uremia occurs when toxic waste products build up in the blood because the kidneys cannot filter them out. This affects brain function and overall health.
Mental changes include confusion, difficulty concentrating, and memory problems. Some patients develop seizures or fall into a coma if uremia becomes severe. Brain fog and decreased mental function[1] are common early signs.
Physical symptoms of uremia include:
- Severe nausea and vomiting
- Loss of appetite
- Metallic taste in the mouth
- Bad breath with a urine-like smell
- Severe itching all over the body
Nerve damage in the arms and legs[7] causes numbness, tingling, and muscle weakness. This makes walking and daily activities difficult.
Without dialysis or kidney transplant, uremia becomes life-threatening as toxins continue building up in the bloodstream.
Diagnosis and Monitoring of Kidney Failure
Doctors use specific blood and urine tests to detect kidney failure, with the estimated glomerular filtration rate being the most important measurement. A nephrologist typically leads the diagnosis process and helps track how quickly kidney function declines over time.
Laboratory and Imaging Tests
Blood and urine tests can check for signs of kidney disease[4], with several key measurements helping doctors assess kidney function.
The estimated glomerular filtration rate (eGFR) is the most important test. This blood test measures how well the kidneys filter waste from the blood. Normal eGFR ranges from 90-120 mL/min/1.73m².
People with kidney failure have an eGFR of less than 15[4] for three months or more. This low number means the kidneys have lost 85-90% of their normal function.
Other important tests include:
- Serum creatinine levels
- Blood urea nitrogen (BUN)
- Urine protein levels
- Electrolyte measurements
Doctors may also order imaging tests like ultrasounds or CT scans. These tests show the size and shape of the kidneys. They can reveal blockages, stones, or other structural problems.
Role of Nephrologists in Diagnosis
A nephrologist is a doctor who specializes in kidney diseases. Primary care doctors often refer patients to nephrologists when kidney problems are suspected.
Nephrologists have advanced training in kidney function and disease. They understand how to interpret complex test results and recognize early warning signs.
These specialists create treatment plans based on the patient’s specific condition. They also coordinate care with other doctors when kidney disease affects other body systems.
Nephrologists typically:
- Perform kidney biopsies when needed
- Adjust medications that affect kidney function
- Monitor disease progression over time
- Prepare patients for dialysis or transplant
Tracking Progression and Staging
Kidney disease has five stages based on eGFR measurements. Stage 1 shows mild damage with normal or high eGFR. Stage 5 represents kidney failure.
Doctors track how quickly eGFR declines over months and years. A steady drop in eGFR indicates worsening kidney function.
The five stages are:
- Stage 1: eGFR 90+ (normal with kidney damage)
- Stage 2: eGFR 60-89 (mild decrease)
- Stage 3: eGFR 30-59 (moderate decrease)
- Stage 4: eGFR 15-29 (severe decrease)
- Stage 5: eGFR under 15 (kidney failure)
Regular monitoring helps doctors predict when patients might need dialysis or transplant. Most people need these treatments when they reach Stage 5.
Blood tests are usually done every 3-6 months in early stages. Testing becomes more frequent as kidney function worsens.
Causes and Risk Factors for Kidney Failure
Several medical conditions and external factors can damage the kidneys over time or cause sudden failure. Diabetes is the most common cause of kidney failure[9], while high blood pressure ranks as the second leading cause.
Diabetes and Hypertension
Diabetes is the leading risk factor for kidney disease and the most common cause of kidney failure[9]. High blood sugar levels damage the small blood vessels in the kidneys. This damage reduces the kidneys’ ability to filter waste properly.
Over many years, diabetes causes the filtering units to thicken and scar. The kidneys work harder to clean the blood. Eventually, they begin to leak protein into the urine.
High blood pressure creates the second most common pathway to kidney failure. Uncontrolled blood pressure damages blood vessels throughout the kidneys. This damage makes it harder for the kidneys to remove waste and extra fluid.
The relationship works both ways. Damaged kidneys cannot regulate blood pressure well. This creates a cycle where high blood pressure worsens kidney damage.
Key risk factors include:
- Type 1 or Type 2 diabetes lasting more than 10 years
- Blood pressure consistently above 140/90 mmHg
- Family history of kidney disease
- Poor blood sugar control
Other Medical Conditions and Infections
Several diseases can attack the kidneys directly. Polycystic kidney disease causes fluid-filled cysts to grow in the kidneys. These cysts slowly replace healthy kidney tissue.
Glomerulonephritis inflames the kidney’s filtering units. This condition can develop from infections like strep throat. It can also result from autoimmune diseases.
Kidney infections that spread from the bladder can cause permanent damage. Repeated infections create scar tissue that reduces kidney function.
Other conditions that increase risk include:
- Lupus and other autoimmune diseases
- Heart disease and stroke
- Hepatitis B and C infections
- HIV/AIDS
Genetic factors play a role in some cases. People with family members who have kidney disease face higher risks. Certain ethnic groups also show increased susceptibility.
Acute Causes and Medication Risks
Acute kidney injury can happen suddenly and progress to permanent failure. Severe dehydration, blood loss, or shock can stop blood flow to the kidneys. Without adequate blood supply, kidney tissue dies quickly.
Medications pose significant risks when used long-term or in high doses. Diuretics help remove excess fluid but can strain the kidneys when overused. They can cause dehydration and electrolyte imbalances.
Pain medications called NSAIDs reduce blood flow to the kidneys. Regular use of ibuprofen, naproxen, or similar drugs increases failure risk.
Other medication risks include:
- Certain antibiotics in high doses
- Chemotherapy drugs
- Heart medications like ACE inhibitors (when combined with dehydration)
- Contrast dyes used in medical imaging
Toxic exposure from heavy metals, solvents, or illegal drugs can destroy kidney tissue rapidly. Heroin and cocaine use significantly increases the risk of sudden kidney failure.
Treatment Options for Kidney Failure
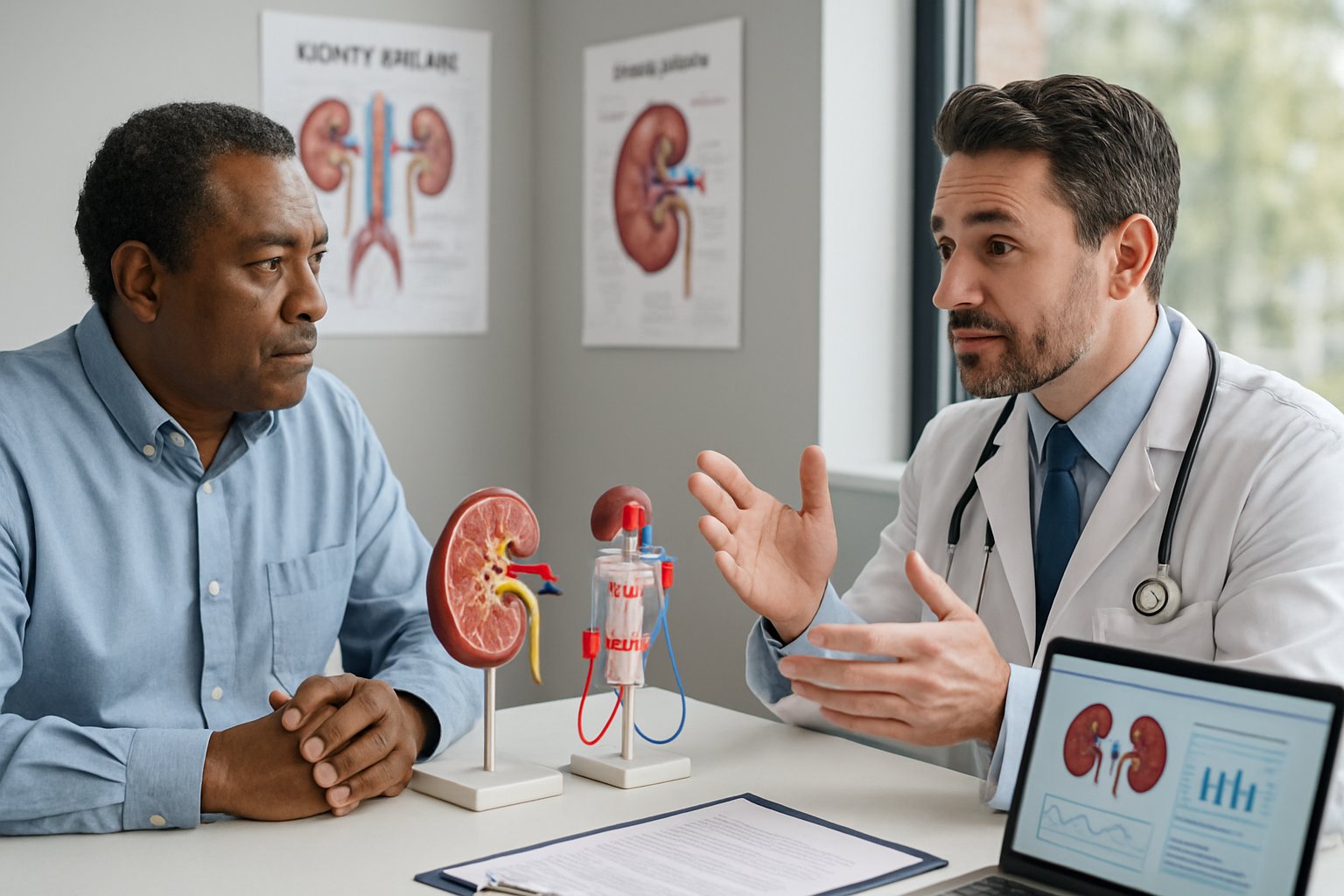
When kidneys fail, patients have several treatment choices for kidney failure[10] including two types of dialysis and transplant surgery. Some patients may also benefit from medications and supportive care to manage symptoms.
Hemodialysis and Peritoneal Dialysis
Hemodialysis uses an artificial kidney machine to filter blood[10] outside the body. Patients visit a dialysis center three times per week for 3-4 hour sessions.
During treatment, blood flows through soft tubes to a special filter called a dialyzer. The machine removes waste and extra fluid before returning clean blood to the patient’s body.
Peritoneal dialysis works differently by cleaning blood inside the body. A cleansing solution enters the abdomen through a soft tube called a PD catheter.
The belly’s lining acts as a natural filter. Waste and fluid move from blood into the cleaning solution. Patients can do this home-based dialysis treatment[10] at work, school, or while traveling.
Key differences between dialysis types:
| Treatment | Location | Frequency | Duration |
|---|---|---|---|
| Hemodialysis | Dialysis center or home | 3x per week | 3-4 hours |
| Peritoneal dialysis | Home/anywhere | Daily | Multiple short sessions |
Kidney Transplant Surgery
A kidney transplant places a healthy kidney[10] from another person into the patient’s body. The donor kidney can come from someone who died or a living donor.
Living donors may be family members, spouses, friends, or generous strangers. The surgery replaces kidney function but requires lifelong care and medication.
Transplant patients must take anti-rejection drugs to prevent their immune system from attacking the new kidney. These medications have side effects and increase infection risk.
Transplant benefits include:
- No need for regular dialysis
- Better quality of life
- Improved energy levels
- More freedom to travel
However, transplants are treatments, not cures. Patients need regular medical checkups and must protect their new kidney carefully.
Medications and Symptom Management
Doctors prescribe medications to treat kidney failure symptoms[1] like fatigue, nausea, and swelling. Blood pressure medications help protect remaining kidney function.
Phosphate binders prevent dangerous mineral buildup in the blood. Patients may need iron supplements or medications to help make red blood cells.
Common medications include:
- Blood pressure drugs (ACE inhibitors, ARBs)
- Phosphate binders
- Vitamin D supplements
- Anemia medications
Dietary changes work alongside medications. Patients often limit protein, sodium, potassium, and phosphorus intake based on their treatment type.
Conservative and Supportive Care Approaches
Some patients choose conservative care instead of dialysis or transplant. This approach focuses on comfort and quality of life rather than extending life.
Conservative care includes pain management, symptom control, and emotional support. Patients work with palliative care teams to stay comfortable at home.
Supportive care services:
- Nutritional counseling
- Social work support
- Mental health counseling
- Pain management
This option works best for elderly patients or those with multiple serious health problems. Families receive guidance and support throughout the process.
Patients can change their mind and start dialysis or pursue transplant later if they choose.
Diet, Nutrition, and Lifestyle Adjustments
When kidneys start to fail, patients must make significant changes to their diet and daily habits. These adjustments help control mineral levels, reduce strain on damaged kidneys, and maintain overall health during kidney failure.
Dietary Guidelines and Fluid Restrictions
People with kidney failure need to follow strict dietary rules. The kidneys can no longer filter waste properly, so certain foods become dangerous.
Protein intake requires careful balance. Dialysis patients may need more protein[11] than before treatment started. Good protein sources include eggs, chicken, fish, and lean meats.
Phosphorus control becomes critical as kidney function declines. High phosphorus levels cause bone disease and heart problems[11]. Patients must limit dairy products, nuts, beans, and dark sodas.
Potassium management prevents dangerous heart rhythms. Too much or too little potassium in blood can be dangerous[11]. Bananas, oranges, potatoes, and tomatoes contain high potassium levels.
Sodium restriction helps control blood pressure and fluid buildup. Patients should avoid processed foods, canned soups, and restaurant meals. Reading food labels becomes essential for tracking sodium intake.
Fluid limits prevent dangerous swelling and breathing problems. Fluid includes ice, beverages, soups, and foods that melt at room temperature[11]. Weight gain between dialysis treatments shows excess fluid retention.
Nutritional Support from a Dietitian
Working with a kidney specialist dietitian provides essential guidance for managing complex dietary needs. These experts understand how kidney failure affects nutrition requirements.
A dietitian will track what patients eat each day. They create meal plans that provide proper amounts of protein, calories, vitamins, and minerals. Dietitians help ensure patients get the right nutrients while avoiding harmful substances[11].
Vitamin and mineral supplements often become necessary. Kidney disease changes how the body processes these nutrients. Only take vitamins that healthcare professionals recommend, as some can harm kidney patients[11].
Appetite problems frequently occur during kidney failure. Nutritional supplements like drinks, bars, and puddings help patients get needed calories[11]. Some supplements are made specifically for kidney patients.
Regular nutrition monitoring through blood tests checks albumin levels and protein intake. These tests show if dietary changes are working properly.
Importance of Physical Activity
Exercise helps kidney failure patients maintain strength and energy levels. Physical activity supports overall health management alongside medical treatments[12].
Regular movement helps control blood pressure and diabetes. Both conditions can worsen kidney damage if left unmanaged. Exercise also improves heart health, which becomes more important as kidney function declines.
Muscle maintenance requires consistent physical activity. Kidney failure often causes muscle wasting and weakness. Simple exercises like walking, stretching, and light weight training help preserve muscle mass.
Energy levels improve with regular exercise routines. Many kidney patients feel tired and weak. Gentle physical activity actually increases energy over time rather than depleting it.
Patients should work with their healthcare team to create safe exercise plans. Activity levels may need adjustment based on treatment schedules and energy levels. Starting slowly and building gradually prevents injury and burnout.
Living with Kidney Failure and Prognosis
People with kidney failure need ongoing medical care to manage symptoms and prevent serious health problems. Treatment options like dialysis can extend life expectancy[13] by up to 10 years or more, while kidney transplants offer the best long-term outcomes.
Managing Symptoms and Quality of Life
Kidney failure causes several symptoms that affect daily life. Patients often experience fatigue, nausea, swelling, and changes in urination patterns.
Common symptoms include:
- Extreme tiredness and weakness
- Swelling in legs, ankles, and face
- Nausea and vomiting
- Shortness of breath
- Brain fog and confusion
Regular dialysis helps control many of these symptoms. Hemodialysis typically requires three sessions per week, each lasting four hours. Peritoneal dialysis can be done at home but requires multiple daily exchanges.
Patients may feel tired after starting dialysis, but many report feeling better able to maintain normal routines. Dietary changes help manage fluid buildup and toxin levels. Most people need to limit salt, potassium, and phosphorus in their diet.
Physical activity remains important when possible. Light exercise can help maintain strength and improve mood.
Prevention of Complications and Infections
Kidney failure complications include fluid retention, anemia, and bone or heart disease[13]. Preventing these problems requires careful monitoring and treatment.
Key prevention strategies:
| Complication | Prevention Method |
|---|---|
| Infections | Keep dialysis access sites clean |
| Heart disease | Control blood pressure and fluid |
| Bone disease | Take phosphorus binders |
| Anemia | Receive iron and EPO injections |
Dialysis patients face higher infection risks. The access points for hemodialysis need proper care and cleaning. Peritoneal dialysis patients must use sterile techniques during fluid exchanges.
Regular blood tests track important levels like hemoglobin, calcium, and phosphorus. Medications help control these levels when diet alone is not enough.
Vaccinations become more important with kidney failure. Patients should get flu shots and other recommended vaccines to prevent serious illness.
Long-Term Outlook and Life Expectancy
Without dialysis or transplant, life expectancy ranges from days to weeks[13]. Treatment options significantly improve these outcomes.
Life expectancy with treatment:
- Dialysis: Can extend life by 10+ years
- Transplant: 10-15 years longer than dialysis
- Living donor kidney: Lasts 12-20 years
- Deceased donor kidney: Lasts 8-12 years
People with kidney transplants live longer than those on dialysis[13]. Even patients as old as 75 benefit from transplants, living an average of four more years than those on dialysis.
Not everyone qualifies for transplant surgery. Age, other health conditions, and overall fitness affect eligibility. The transplant waiting list can be long, especially for deceased donor kidneys.
Younger patients generally have better outcomes with both dialysis and transplants. However, many older adults also do well with proper treatment and care.
Frequently Asked Questions
People with kidney problems often have questions about symptoms, causes, and what to expect. Understanding the early warning signs, damage causes, prevention methods, and survival rates helps patients make informed decisions about their care.
What are the initial symptoms indicating potential kidney problems?
Many people experience few or no symptoms in the early stages of kidney disease. The kidneys can still suffer damage even when a person feels fine.
Early warning signs include extreme tiredness and nausea. People may also notice confusion or trouble concentrating.
Swelling around the hands, ankles, or face is another common sign. Changes in how often someone urinates can also indicate kidney problems.
Other symptoms include muscle cramps and dry or itchy skin. Food may taste metallic, and appetite often decreases as kidney function declines.
How can damage to the kidneys occur?
Diabetes and high blood pressure are the most common causes[1] of chronic kidney disease and kidney failure. Unmanaged diabetes leads to high blood sugar levels that damage kidney tissue over time.
High blood pressure forces blood through vessels with extra force. This constant pressure damages the delicate kidney tissue without proper treatment.
Inherited conditions like polycystic kidney disease cause fluid-filled cysts to grow inside the kidneys. Autoimmune diseases like lupus can also attack kidney tissue.
Acute kidney damage can happen quickly from certain medications or severe dehydration. Urinary tract blockages and untreated heart or liver disease can also cause sudden kidney failure.
What strategies can prevent kidney failure?
Managing diabetes and blood pressure prevents most kidney damage. People with diabetes should keep blood sugar levels within target ranges set by their doctor.
Regular blood pressure monitoring and medication help protect kidney function. A healthy diet low in sodium and processed foods supports kidney health.
Staying hydrated helps kidneys filter waste properly. People should avoid overuse of pain medications like NSAIDs that can damage kidneys over time.
Regular check-ups allow doctors to catch kidney problems early. Blood and urine tests can detect kidney damage before symptoms appear.
What are specific kidney disease symptoms experienced by females?
Women experience the same kidney failure symptoms as men. These include fatigue, nausea, swelling, and changes in urination patterns.
Some women may notice symptoms during pregnancy if they have underlying kidney disease. Swelling during pregnancy can sometimes mask kidney-related fluid retention.
Women with autoimmune diseases like lupus face higher risks for kidney damage. They should monitor for symptoms like joint pain combined with kidney warning signs.
Urinary tract infections are more common in women and can sometimes lead to kidney problems if left untreated.
What are the symptoms associated with stage 5 kidney disease?
Stage 5 kidney disease means the kidneys function at less than 15% of normal capacity. Symptoms become severe and affect daily life significantly.
Extreme fatigue makes it difficult to perform normal activities. Nausea and vomiting become frequent and interfere with eating.
Swelling becomes pronounced throughout the body, especially in legs and face. Breathing may become difficult due to fluid buildup in the lungs.
Mental confusion increases as waste products build up in the blood. Muscle cramps and bone pain become more severe and frequent.
How long can a person survive with end-stage kidney failure without dialysis?
Survival time varies greatly depending on remaining kidney function and overall health. Some people may survive weeks to months without treatment.
End-stage renal failure can lead to death[1] without proper medical intervention. The kidneys cannot remove enough waste products and excess fluid from the body.
Younger, healthier individuals may survive longer than older people with multiple health conditions. The rate of kidney function decline also affects survival time.
Most doctors recommend starting dialysis or considering transplant when kidneys function below 10-15% capacity. These treatments can significantly extend life and improve quality of living.
References
- Kidney Failure: Stages, ESRD, Causes, Symptoms & Treatment. https://my.clevelandclinic.org/health/diseases/17689-kidney-failure Accessed October 21, 2025
- How Your Kidneys Work. https://www.kidney.org/kidney-topics/kidney-function Accessed October 21, 2025
- Kidney Failure Causes, Symptoms, and Treatments. https://www.upmc.com/services/kidney-disease/conditions/kidney-failure Accessed October 21, 2025
- Kidney failure (ESRD). https://www.kidney.org/kidney-topics/kidney-failure Accessed October 21, 2025
- Stages of kidney disease (CKD). https://www.kidneyfund.org/all-about-kidneys/stages-kidney-disease Accessed October 21, 2025
- 15 Symptoms of Kidney Disease. https://lifeoptions.org/learn-about-kidney-disease/kidney-disease-symptoms/ Accessed October 21, 2025
- Content - Health Encyclopedia. https://www.urmc.rochester.edu/encyclopedia/content?ContentTypeID=85&ContentID=P01474 Accessed October 21, 2025
- Health problems caused by kidney disease. https://www.kidneyfund.org/living-kidney-disease/health-problems-caused-kidney-disease Accessed October 21, 2025
- Risk factors. https://www.kidneyfund.org/all-about-kidneys/risk-factors Accessed October 21, 2025
- Choosing A Treatment For Kidney Failure. https://www.kidney.org/kidney-topics/choosing-treatment-kidney-failure Accessed October 21, 2025
- Nutrition and Kidney Failure. https://www.kidney.org/kidney-topics/nutrition-and-kidney-failure Accessed October 21, 2025
- Lifestyle Changes for Kidney Disease. https://nyulangone.org/conditions/kidney-disease/treatments/lifestyle-changes-for-kidney-disease Accessed October 21, 2025
- Kidney Failure Life Expectancy & Prognosis. https://resources.healthgrades.com/right-care/kidney-disease/kidney-failure-prognosis-and-life-expectancy Accessed October 21, 2025
