Most people with low HDL cholesterol don’t experience any symptoms right away. Low HDL cholesterol rarely causes immediate health problems, but it significantly increases the risk of heart attack, stroke, and premature heart disease over time. This makes it a silent threat that many people don’t know they have until serious complications develop.
HDL cholesterol is often called “good” cholesterol because it helps remove harmful cholesterol from the arteries. When HDL levels drop below 40 mg/dL for men or 50 mg/dL for women, the risk of cardiovascular problems increases substantially[1]. The body needs adequate HDL levels to protect against plaque buildup in the arteries.
The good news is that low HDL cholesterol can often be improved through lifestyle changes and medical treatment when necessary. Understanding what causes low HDL levels and how to address them can help prevent serious health complications down the road.
Key Takeaways
- Low HDL cholesterol usually has no symptoms but increases the risk of heart disease and stroke over time
- Regular cholesterol testing is the only way to detect low HDL levels before health problems occur
- Lifestyle changes like exercise, weight loss, and dietary improvements can help raise HDL cholesterol levels
Understanding HDL Cholesterol
HDL cholesterol is a protein particle that removes harmful cholesterol from arteries and transports it to the liver for disposal. Unlike other cholesterol types, higher HDL levels protect against heart disease, with optimal ranges varying by age and gender.
What Is HDL Cholesterol and Its Function
HDL stands for high-density lipoprotein, a protein particle that carries cholesterol through the bloodstream. The particle gets its name from having more protein than fat, making it denser than other lipoproteins.
HDL’s main job involves removing excess cholesterol from artery walls. This process, called cholesterol efflux, prevents dangerous plaque buildup that can block blood flow to the heart and brain.
The protein component apolipoprotein A1 (ApoA1) makes up most of HDL’s structure. ApoA1 helps HDL bind to cells and collect unwanted cholesterol deposits throughout the body.
After collecting cholesterol, HDL transports it back to the liver. The liver then breaks down this cholesterol or converts it into bile acids that help digest fats.
Difference Between HDL, LDL, and Triglycerides
Low-density lipoprotein (LDL) carries cholesterol from the liver to cells throughout the body. When LDL levels get too high, excess cholesterol builds up in artery walls.
Triglycerides are fats that store energy in the body. High triglyceride levels often occur alongside low HDL cholesterol and increase heart disease risk.
A lipid panel measures all three components to assess cardiovascular health:
- HDL cholesterol: Removes cholesterol from arteries
- LDL cholesterol: Delivers cholesterol to cells but can cause blockages
- Triglycerides: Energy storage fats that affect heart health
Total cholesterol combines HDL, LDL, and a portion of triglycerides into one number. However, the individual components provide more useful health information than total cholesterol alone.
Why HDL Is Called ‘Good Cholesterol’
HDL earns the title “good cholesterol”[2] because it actively protects against heart disease. Higher HDL levels reduce the risk of heart attacks and strokes.
The particle works like a cleanup crew, removing dangerous cholesterol deposits from artery walls. This prevents the formation of plaques that can rupture and cause blood clots.
Research shows that HDL cholesterol carries LDL cholesterol away from arteries[3] back to the liver for disposal. This reverse cholesterol transport system keeps arteries clear and flexible.
Unlike LDL cholesterol, which people want to keep low, higher HDL levels provide better protection. Each 1 mg/dL increase in HDL cholesterol can reduce heart disease risk by 2-3%.
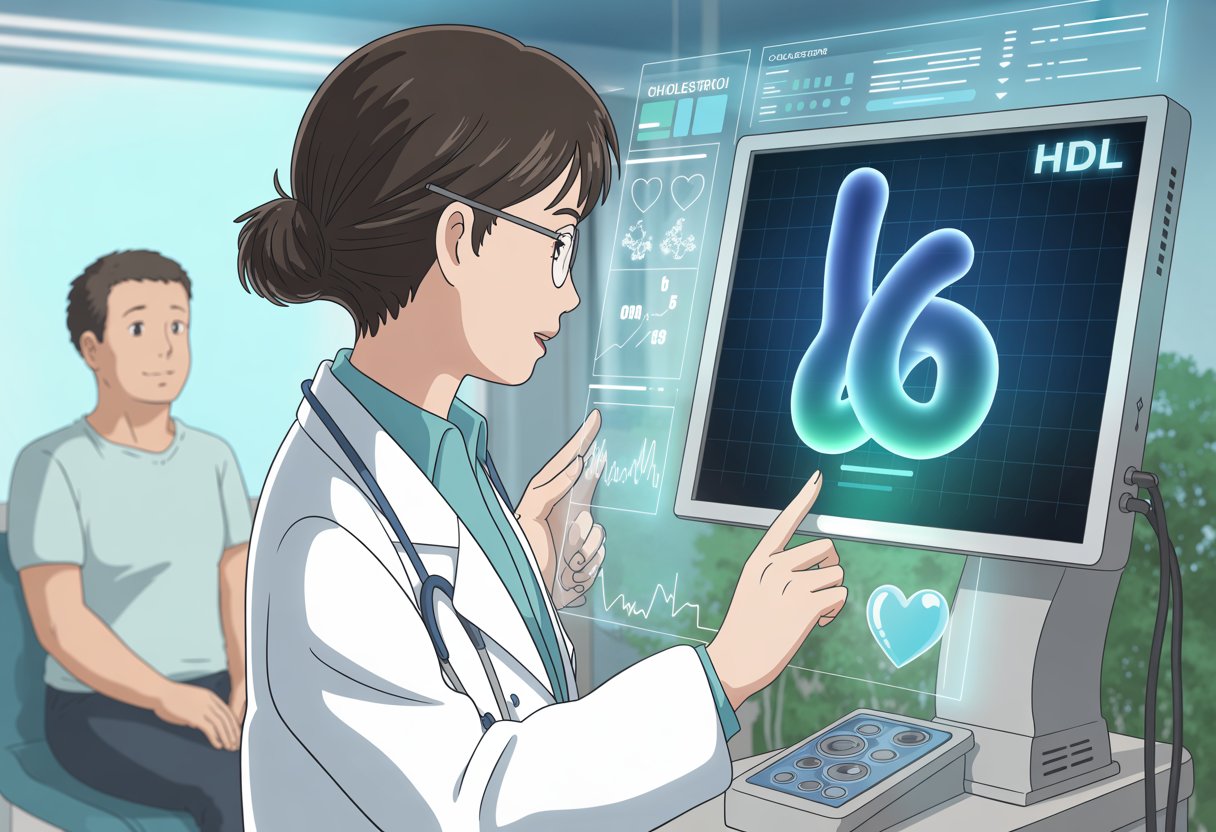
Optimal HDL Cholesterol Levels by Age and Gender
Cholesterol levels vary by age and gender, with women typically having higher HDL than men. Normal HDL ranges from 40 to 80 mg/dL in males and 50 to 80 mg/dL in females[2].
| Age Group | Male HDL Target | Female HDL Target |
|---|---|---|
| 19 and younger | Above 45 mg/dL | Above 45 mg/dL |
| 20 and older | Above 40 mg/dL | Above 50 mg/dL |
Low HDL cholesterol occurs when levels fall below these targets. Men with HDL below 40 mg/dL and women below 50 mg/dL face increased cardiovascular risks.
Doctors use a cholesterol test to measure HDL levels along with other lipoproteins. Regular testing helps identify low HDL cholesterol[1] before serious health problems develop.
Optimal HDL levels above 60 mg/dL provide even greater protection against heart disease for both men and women.
Health Risks of Low HDL Cholesterol
Low HDL cholesterol increases the risk of several serious health conditions. Low HDL levels can lead to cardiovascular disease, stroke, heart attack, and coronary artery disease[1], while also contributing to cognitive decline and metabolic dysfunction.
Cardiovascular Disease and Atherosclerosis Risk
Low HDL cholesterol significantly increases cardiovascular disease risk by reducing the body’s ability to remove harmful cholesterol from artery walls. HDL cholesterol acts as a protective agent that transports cholesterol away from arteries back to the liver for disposal.
When HDL levels drop below optimal ranges, this protective mechanism weakens. Cholesterol accumulates in artery walls more easily, leading to atherosclerosis development.
Atherosclerosis occurs when fatty deposits build up inside arteries, forming plaques. These plaques narrow blood vessels and reduce blood flow to vital organs.
Key cardiovascular risks include:
- Increased plaque formation in arteries
- Reduced endothelial function
- Higher levels of oxidative stress
- Increased inflammation in blood vessels
People with HDL levels below 40 mg/dL for men and 50 mg/dL for women face significantly higher cardiovascular risk. This risk compounds when combined with other factors like high LDL cholesterol or elevated triglycerides.
Heart Attack, Stroke, and Coronary Artery Disease
Low HDL cholesterol directly contributes to life-threatening cardiovascular events. Without adequate HDL levels, there is a higher risk of plaques forming to block arteries[1], which can lead to heart attacks and strokes.
Coronary artery disease develops when plaques narrow the arteries supplying blood to the heart muscle. Premature coronary artery disease occurs before age 55 in males or 65 in females[1] when HDL levels remain consistently low.
Heart attacks happen when coronary arteries become completely blocked. Ischemic strokes occur when blood clots or plaques block arteries leading to the brain.
Critical risks include:
- Sudden cardiac events
- Brain tissue damage from reduced blood flow
- Permanent disability from stroke complications
- Increased mortality risk
The combination of low HDL and other risk factors creates a particularly dangerous situation for cardiovascular health.
Cognitive Decline and Dementia
Research shows connections between low HDL cholesterol and cognitive decline. The brain requires adequate blood flow and cholesterol metabolism for optimal function.
Low HDL levels may contribute to reduced blood flow to brain tissues. This reduction can affect memory, thinking abilities, and overall cognitive performance over time.
Inflammation and oxidative stress associated with poor cholesterol profiles can damage brain cells. These processes may accelerate the development of dementia and other neurodegenerative conditions.
Cognitive risks include:
- Accelerated memory loss
- Reduced processing speed
- Increased dementia risk
- Impaired executive function
The brain’s high cholesterol requirements make proper HDL function essential for maintaining cognitive health throughout aging.
Metabolic Dysfunction and Diabetes
Low HDL cholesterol frequently occurs alongside metabolic dysfunction and diabetes. People diagnosed with diabetes tend to have low HDL levels, especially those with type 2 diabetes[1].
Type 2 diabetes and metabolic syndrome create a cycle where low HDL worsens insulin resistance. This relationship makes blood sugar control more difficult and increases cardiovascular risk.
Insulin resistance reduces the body’s ability to process glucose effectively. Low HDL levels compound this problem by contributing to inflammation and oxidative stress.
Metabolic complications include:
- Worsening insulin resistance
- Poor blood sugar control
- Increased abdominal fat storage
- Higher triglyceride levels
Low HDL levels may increase the risk of peripheral polyneuropathy in people without diabetes[1]. This condition damages nerves outside the brain and spinal cord, causing numbness and pain in hands and feet.
Causes and Risk Factors for Low HDL Cholesterol

Several factors can cause HDL cholesterol levels to drop below healthy ranges. These include rare genetic conditions, excess body weight, poor dietary choices, and harmful lifestyle habits like smoking and lack of exercise.
Genetic Disorders and Rare Causes
Rare genetic mutations can cause severely low HDL levels that run in families. Tangier disease occurs due to mutations in the ABCA1 gene[4], leading to extremely low HDL cholesterol.
Another condition called familial hypoalphalipoproteinemia results from mutations in the APOA1, ABCA1, or LCAT genes. These genetic defects prevent the body from making enough HDL cholesterol.
ApoA1 protein plays a key role in HDL production. When genes affecting ApoA1 don’t work properly, HDL levels drop significantly.
People with these genetic disorders often have HDL levels well below normal ranges. Family history of very low HDL cholesterol may indicate a genetic cause.
Impact of Obesity and Weight
Excess weight directly affects HDL cholesterol levels through changes in blood fats. When people are overweight or have obesity, triglyceride levels increase[4].
Higher triglycerides cause HDL cholesterol to break down faster in the bloodstream. This leads to lower HDL counts over time.
Weight loss can help raise HDL levels back to healthy ranges. Losing just 5% of body weight can improve cholesterol levels[4] in the short term.
Long-term goals include losing 15% of total body weight and keeping it off. Even modest weight reduction helps improve the balance between good and bad cholesterol.
The location of excess weight also matters. People who carry weight around their waist have higher risks for low HDL cholesterol.
Diet and Nutritional Influences
Food choices have a major impact on HDL cholesterol production. Diets high in refined carbohydrates like white bread and sugar cause the liver to make more triglycerides[4], which lowers HDL levels.
Saturated fat from red meat and high-fat dairy products can reduce HDL cholesterol. Trans fats found in processed foods have even stronger negative effects.
Healthy fats help maintain better cholesterol balance. Olive oil, nuts, and other plant-based foods contain fats that support HDL production.
People should limit refined carbohydrates and choose whole grains instead. Low-fat diets may not always help HDL levels if they’re too high in processed carbs.
The best approach includes more fruits, vegetables, and foods with healthy unsaturated fats. These dietary changes can gradually improve HDL cholesterol over several months.
Lifestyle Factors: Smoking and Physical Inactivity
Smoking damages HDL cholesterol through multiple pathways in the body. Tobacco chemicals lower HDL levels in different ways[4], though scientists don’t fully understand all the mechanisms.
Cigarette smoke appears to interfere with proteins needed to build HDL cholesterol. It also affects liver function, which plays a role in cholesterol metabolism.
Smoking cessation can help restore healthier HDL levels over time. Many insurance plans cover quit-smoking programs and medications.
Lack of physical activity contributes to low HDL cholesterol levels. Exercise improves HDL’s ability to remove fatty deposits from arteries[4].
Aerobic exercise and aerobic activity are particularly effective for raising HDL cholesterol. The duration of exercise matters more than intensity[4] for improving HDL levels.
Adults should aim for 150 minutes of moderate exercise or 75 minutes of vigorous activity each week. Regular physical activity helps maintain healthy cholesterol balance long-term.
Medical Conditions and Medications That Affect HDL Levels

Several medical conditions can lower HDL cholesterol levels, with diabetes and metabolic dysfunction being the most common causes. Certain medications like beta-blockers and anabolic steroids also reduce good cholesterol levels.
Diabetes and Insulin Resistance
Type 2 diabetes significantly impacts HDL cholesterol levels through multiple mechanisms. High blood sugar damages the proteins that help make HDL particles work properly.
Insulin resistance is strongly associated with low HDL levels[5]. When cells don’t respond well to insulin, the body produces more insulin to compensate.
This excess insulin changes how the liver processes fats. It increases triglyceride production while reducing HDL cholesterol synthesis.
Common effects of diabetes on HDL:
- HDL levels drop by 10-20% in uncontrolled diabetes
- Small, dense HDL particles form instead of large, protective ones
- HDL function becomes impaired even when levels appear normal
People with metabolic dysfunction often have HDL levels below 40 mg/dL for men and 50 mg/dL for women. Better blood sugar control through medication and lifestyle changes can help raise HDL levels.
Chronic Kidney Disease and Autoimmune Disorders
Chronic kidney disease affects HDL metabolism in several ways. Damaged kidneys cannot filter waste products properly, leading to inflammation throughout the body.
This chronic inflammation interferes with HDL production in the liver. The kidneys also lose important proteins that help maintain healthy cholesterol levels.
Rheumatoid arthritis and other autoimmune disorders create ongoing inflammation. This inflammatory state reduces HDL cholesterol levels and changes HDL particle structure.
Key inflammatory effects:
- Cytokines block HDL synthesis
- Existing HDL particles become less effective
- Oxidative stress damages cholesterol transport systems
Treating the underlying kidney disease or autoimmune condition often helps improve HDL levels. Anti-inflammatory medications may also provide benefits for cholesterol metabolism.
Hormonal Imbalances and Endocrine Causes
Hormones play a major role in controlling HDL cholesterol levels. Low testosterone in men is linked to reduced HDL production.
Thyroid disorders affect cholesterol metabolism significantly. Hypothyroidism slows down the processes that create and maintain HDL particles.
Hormonal factors affecting HDL:
- Low testosterone: Reduces HDL by 15-25%
- Hypothyroidism: Decreases HDL synthesis
- PCOS: Creates insulin resistance and metabolic dysfunction
- Menopause: Natural estrogen decline lowers HDL levels
Women typically have higher HDL levels than men due to estrogen’s protective effects. After menopause, HDL levels often drop as estrogen production decreases.
Hormone replacement therapy can raise HDL levels in postmenopausal women. However, doctors must weigh the cardiovascular benefits against potential risks.
Medications and Their Effects on HDL
Many common medications can lower HDL cholesterol levels as a side effect. Beta-blockers used for blood pressure and heart conditions[5] can reduce HDL by 10-15%.
Anabolic steroids significantly suppress HDL production. These medications alter liver metabolism and can drop HDL levels by 50% or more.
Progesterone and other progestational drugs also lower HDL cholesterol. Birth control pills containing certain progestins may affect cholesterol levels.
Medications that lower HDL:
| Medication Type | HDL Reduction | Mechanism |
|---|---|---|
| Beta-blockers | 10-15% | Reduced liver synthesis |
| Anabolic steroids | 30-50% | Altered liver metabolism |
| Progestins | 5-20% | Hormonal pathway changes |
Some medications can help raise HDL levels. Niacin is highly effective but may cause side effects like flushing. Fibrates work well when triglyceride levels are also high.
Statins primarily lower LDL cholesterol but provide modest HDL increases of 5-10%. Patients should discuss medication effects on cholesterol with their healthcare providers.
Diagnosing and Monitoring Low HDL Cholesterol
Testing for low HDL cholesterol involves routine lipid panels that measure multiple cholesterol components. Healthcare providers typically evaluate HDL levels alongside other lipid markers and inflammatory indicators to assess cardiovascular risk.
When to Test HDL Cholesterol
Adults should have their first cholesterol test by age 20, with repeat testing every 4-5 years if results are normal. More frequent testing is needed for people with risk factors.
High-risk individuals require annual testing:
- Family history of heart disease
- Diabetes or prediabetes
- High blood pressure
- Obesity
- Smoking history
People taking cholesterol medications need testing every 3-6 months initially. Once levels stabilize, testing can occur every 6-12 months.
The lipid panel requires a 9-12 hour fast for accurate triglyceride measurements. HDL cholesterol levels remain stable without fasting, but complete lipid testing provides better cardiovascular risk assessment.
Interpreting Lipid Panel Results
A standard lipid panel measures four key components that work together to determine heart disease risk.
HDL Cholesterol Levels:
- Optimal: 60 mg/dL or higher
- Acceptable: 40-59 mg/dL for men, 50-59 mg/dL for women
- Low: Below 40 mg/dL for men, below 50 mg/dL for women
Complete Lipid Profile Targets:
- Total cholesterol: Less than 200 mg/dL
- LDL cholesterol: Less than 100 mg/dL
- Triglycerides: Less than 150 mg/dL
The ratio of total cholesterol to HDL cholesterol provides additional insight. A ratio below 4:1 indicates lower cardiovascular risk.
Low HDL cholesterol symptoms[1] are uncommon, making regular testing essential for detection.
Associated Biomarkers and Inflammatory Markers
Healthcare providers often measure additional markers alongside standard lipid testing to better assess cardiovascular risk and lipid metabolism.
Advanced Lipid Testing:
- Apolipoprotein A-I (the main protein in HDL)
- HDL particle size and number
- Lipoprotein(a) levels
Inflammatory Markers:
- C-reactive protein (CRP)
- Interleukin-6
- Fibrinogen levels
These inflammatory markers help identify patients with increased cardiovascular risk despite normal cholesterol levels. High inflammation combined with low HDL cholesterol significantly increases heart disease risk.
Metabolic Assessment:
- Fasting glucose levels
- Hemoglobin A1C
- Insulin resistance markers
Low HDL cholesterol often occurs with metabolic syndrome. This condition combines multiple risk factors including high triglycerides, elevated blood pressure, and increased waist circumference.
Strategies for Improving Low HDL Cholesterol

Raising HDL cholesterol requires a combination of proven lifestyle modifications and targeted medical interventions. Evidence-based approaches include dietary changes, regular physical activity, smoking cessation, and specific medications when needed.
Lifestyle Changes: Diet, Exercise, and Weight Management
Dietary modifications play a crucial role in boosting HDL levels. Heart-healthy eating patterns[6] focus on omega-3 fatty acids found in fatty fish like salmon and sardines. These should be consumed at least twice weekly.
Plant-based foods provide essential nutrients for HDL production. Nuts, especially almonds and walnuts, contain healthy fats that support good cholesterol. Olive oil serves as an excellent replacement for saturated fats in cooking and salad dressings.
Regular physical activity directly increases HDL cholesterol levels. Moderate to high-intensity exercise[6] produces measurable improvements in just weeks. Adults should aim for 150 minutes of moderate exercise or 75 minutes of vigorous activity weekly.
Activities include:
- Brisk walking or jogging
- Swimming or cycling
- Weight training
- Dancing or sports
Weight management significantly impacts cholesterol levels. Losing just 5-10% of body weight[6] can improve both HDL and LDL numbers. Maintaining a healthy weight reduces cardiovascular risk and supports overall heart health.
Smoking Cessation and Reducing Alcohol Intake
Smoking cessation provides rapid HDL improvements. HDL levels typically rise within three weeks[6] of quitting tobacco use. Smoking damages blood vessels and reduces the body’s ability to produce protective cholesterol.
Vaping products also negatively affect HDL levels. Complete tobacco cessation offers the greatest benefits for cholesterol management and cardiovascular health.
Moderate alcohol consumption may slightly increase HDL in some individuals. However, alcohol carries significant health risks including liver damage, addiction, and increased triglycerides. Healthcare providers rarely recommend alcohol specifically for cholesterol improvement due to these substantial risks.
Medical and Pharmacological Approaches
Statins remain the first-line treatment for cholesterol management. While primarily designed to lower LDL cholesterol, some statins provide modest HDL increases. These medications work by blocking cholesterol production in the liver.
Niacin effectively raises HDL cholesterol levels by 15-35%. However, side effects include flushing, itching, and potential liver problems. Extended-release formulations reduce some adverse effects but require careful monitoring.
Fibrates target triglycerides while modestly increasing HDL. These medications work best in patients with very high triglyceride levels. Common options include fenofibrate and gemfibrozil.
| Medication Type | HDL Increase | Primary Use |
|---|---|---|
| Statins | 5-10% | LDL reduction |
| Niacin | 15-35% | HDL elevation |
| Fibrates | 10-20% | Triglyceride reduction |
Emerging Research and Novel Therapies
CETP inhibitors represent promising new treatments that significantly raise HDL levels. These medications block a protein that transfers cholesterol between lipoproteins. Clinical trials show HDL increases of 100% or more with certain compounds.
Gene therapy approaches target specific genetic variants affecting HDL metabolism. Research focuses on enhancing the body’s natural HDL production pathways through targeted interventions.
Advanced nutraceuticals including specific plant sterols and concentrated omega-3 formulations show potential for HDL improvement. These supplements require further study to establish optimal dosing and long-term safety profiles.
Personalized medicine approaches analyze individual genetic profiles to predict treatment responses. This emerging field helps healthcare providers select the most effective interventions for each patient’s unique cholesterol metabolism.
Frequently Asked Questions
Low HDL cholesterol raises specific health risks and affects men and women differently. Simple lifestyle changes and medical treatments can help improve HDL levels.
What are the risks associated with low HDL cholesterol levels?
Low HDL cholesterol increases the risk of several serious health problems. Having too little good cholesterol can lead to stroke, heart attack, and premature coronary artery disease[1].
People with low HDL face higher chances of developing blocked arteries. Plaques form more easily in blood vessels when HDL levels drop below normal ranges.
Low HDL also connects to peripheral nerve damage called polyneuropathy. This condition can affect people even without diabetes when their HDL stays too low.
Can low HDL cholesterol affect women differently from men?
Women need higher HDL levels than men to maintain good health. Females age 20 and older should keep HDL above 50 mg/dL, while males need levels above 40 mg/dL.
Women typically have naturally higher HDL levels than men. However, certain birth control pills containing progestins can lower HDL in women.
Heart disease risks from low HDL may appear earlier in men. Premature coronary artery disease occurs before age 55 in males but before age 65 in females.
What lifestyle changes can lead to an increase in HDL cholesterol?
Regular exercise helps boost HDL cholesterol levels significantly. People should aim for at least 30 minutes of physical activity five days per week.
Weight loss improves HDL levels in overweight individuals. Even modest weight reduction can make a meaningful difference in cholesterol numbers.
Quitting smoking raises HDL cholesterol quickly. Tobacco use directly lowers good cholesterol levels and stops this beneficial effect.
Dietary changes support higher HDL levels. Eating olive oil, nuts like almonds and walnuts, and foods with niacin can help improve cholesterol.
What medical treatments are available for low HDL cholesterol?
Doctors usually focus on lowering bad LDL cholesterol first with statin medications. These drugs provide more proven benefits than treatments specifically targeting HDL levels.
Healthcare providers may review current medications that could lower HDL. Beta blockers and certain birth control pills can reduce good cholesterol levels.
Some people benefit from niacin supplements to raise HDL. However, doctors must monitor patients carefully due to potential side effects.
Are there specific symptoms that indicate HDL cholesterol levels are too low?
Most people with low HDL experience no immediate symptoms. Having too little good cholesterol causes no immediate health problems[1].
Regular blood tests provide the only reliable way to detect low HDL. People may not realize their levels are low until a serious health event occurs.
Rare genetic conditions like Tangier disease can cause extremely low HDL with visible symptoms. These include yellowish skin deposits, enlarged organs, and eye changes.
What potential health conditions are linked to low HDL cholesterol?
Diabetes and low HDL often occur together, especially in type 2 diabetes. Poor blood sugar control, obesity, and lack of exercise contribute to both conditions.
Heart disease represents the primary concern with low HDL levels. Coronary artery disease develops more easily when good cholesterol stays below recommended levels.
Research suggests low HDL may connect to other health problems. Scientists study links between low HDL and conditions like macular degeneration and dementia.
Metabolic syndrome frequently includes low HDL as one component. This cluster of conditions raises the risk of heart disease, stroke, and diabetes.
References
- the risk of cardiovascular problems increases substantially. https://www.verywellhealth.com/low-hdl-symptoms-signs-symptoms-and-complications-5188643 Accessed October 28, 2025
- HDL: Why It’s “Good” Cholesterol. https://my.clevelandclinic.org/health/articles/24395-hdl-cholesterol Accessed October 28, 2025
- Document Not Found. https://healthlibrary.osfhealthcare.org/MultimediaRoom/88,p11228 Accessed October 28, 2025
- Tangier disease occurs due to mutations in the ABCA1 gene. https://www.verywellhealth.com/what-causes-low-hdl-cholesterol-levels-698078 Accessed October 28, 2025
- Low HDL Cholesterol (Hypoalphalipoproteinemia) Treatment & Management: Medical Care, Surgical Care, Consultations. https://emedicine.medscape.com/article/127943-treatment Accessed October 28, 2025
- 5 Ways To Increase HDL. https://health.clevelandclinic.org/hdl-is-it-possible-to-raise-your-good-cholesterol-2 Accessed October 28, 2025
