A low platelet count can lead to serious bleeding problems that affect daily life and overall health. Platelets are tiny blood cells that help form clots to stop bleeding when you get cut or injured.
When platelet counts drop below 150,000 per microliter of blood, a person may experience easy bruising, longer bleeding times, and in severe cases, dangerous internal bleeding. This condition, called thrombocytopenia, occurs when blood has too few platelets[1] and can happen for many different reasons.
Understanding what causes low platelets and recognizing the warning signs can help people get the right treatment quickly. The severity of symptoms depends on how low the count drops, with some cases requiring immediate medical attention while others need only careful monitoring.
Key Takeaways
- Low platelet counts cause easy bruising, excessive bleeding, and tiny red spots on the skin
- Common causes include viral infections, certain medications, autoimmune conditions, and bone marrow problems
- Treatment options range from medication changes to steroids, platelet transfusions, or spleen removal depending on the underlying cause
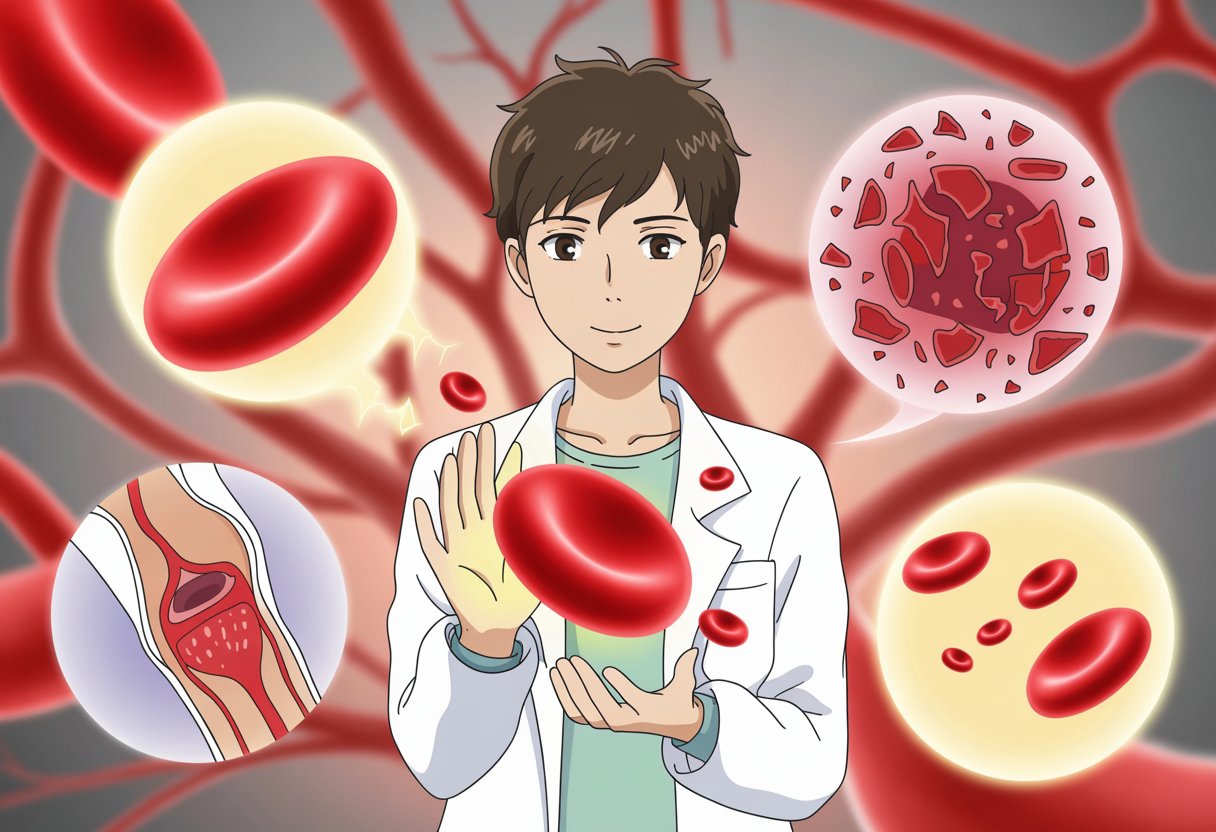
Understanding Platelet Count and Thrombocytopenia
Platelets are tiny blood cells that help stop bleeding by forming clots when injuries occur. Thrombocytopenia occurs when blood has too few platelets[1], which can lead to increased bleeding and bruising.
What Are Platelets and Thrombocytes?
Platelets and thrombocytes are two names for the same blood cells. These tiny, disc-shaped cells form in the bone marrow.
They measure only 2-3 micrometers across, making them the smallest cells in blood. The bone marrow produces about 100 billion new platelets every day.
Platelets live for about 7-10 days in the bloodstream before the body removes them. The spleen stores about one-third of all platelets at any given time.
When blood vessels get damaged, platelets become sticky and clump together. This process helps seal wounds and prevents excessive blood loss.
Normal Platelet Count Ranges
A normal platelet count ranges from 150,000 to 450,000 platelets per microliter[1] of blood. Doctors measure platelet count through a complete blood count (CBC) test.
Platelet Count Categories:
| Range | Classification | Risk Level |
|---|---|---|
| 150,000-450,000 | Normal | No increased risk |
| Below 150,000 | Mildly low | Mild bleeding risk |
| Below 50,000 | Moderately low | Increased bleeding risk |
| 10,000-20,000 or lower | Severely low | High bleeding risk |
The CBC test is a common blood test that measures different blood cell types. It provides doctors with important information about overall blood health.
People with counts below 150,000 have thrombocytopenia. The severity depends on how low the count drops.
How Platelets Function in Blood Clotting
Platelets play a crucial role in forming blood clots to stop bleeding. When a blood vessel gets cut or damaged, platelets rush to the area.
First, platelets stick to the damaged blood vessel wall. This process is called adhesion and happens within seconds of injury.
Next, platelets change shape and become sticky. They send out signals that attract more platelets to the injury site.
The platelets clump together to form a plug that temporarily stops bleeding. This initial plug is soft and needs strengthening.
Platelets release chemicals that activate the clotting process. These chemicals help create fibrin threads that make the blood clot stronger and more permanent.
Without enough platelets, this clotting process becomes slower and less effective. People with low platelet counts may bleed longer from cuts or bruise more easily.
Signs and Symptoms of Low Platelet Count

Low platelet counts cause bleeding and bruising problems because blood cannot clot properly. People may notice small red spots on their skin, get tired easily, and have bleeding that lasts longer than normal.
Bleeding and Bruising
People with low platelets bruise much easier than normal. Small bumps that would not usually cause bruises can leave large, dark marks on the skin.
The bruises often appear without any clear cause. They may show up on arms, legs, or other body parts even from light pressure.
Prolonged bleeding happens when cuts or scrapes take much longer to stop bleeding. A small cut that normally stops bleeding in a few minutes might bleed for 15-30 minutes or longer.
Bleeding from the gums is common, especially when brushing teeth. The gums may bleed easily and take time to stop.
Some people notice blood in their urine or stool. This internal bleeding can be serious and needs medical attention right away.
Petechiae and Purpura
Petechiae are tiny red or purple spots that appear on the skin. These spots are smaller than a pinhead and look like small dots.
They often show up on the legs, ankles, and feet first. The spots do not go away when pressed and cannot be felt when touched.
Purpura are larger purple or red patches on the skin. These patches are bigger than petechiae and can be several inches wide.
Both petechiae and purpura happen because small blood vessels under the skin leak blood. Without enough platelets, the body cannot stop these tiny bleeds.
These skin changes are often the first signs of thrombocytopenia that people notice.
Fatigue and Weakness
Fatigue from low platelets feels different from normal tiredness. People may feel extremely tired even after getting enough sleep.
This tiredness happens because the body works harder when it has bleeding problems. Internal bleeding, even small amounts, can make people feel weak.
Some people feel dizzy or lightheaded, especially when standing up quickly. This can happen if there is ongoing bleeding inside the body.
The weakness may get worse with physical activity. Simple tasks like climbing stairs or carrying groceries may feel much harder than usual.
Nosebleeds and Heavy Menstrual Bleeding
Nosebleeds become more frequent and harder to stop with low platelets. A normal nosebleed might stop in 5-10 minutes, but with thrombocytopenia it could last 20-30 minutes or longer.
The nosebleeds may start without any cause like dry air or nose picking. They can happen several times a week or even daily.
Heavy menstrual bleeding affects women with low platelets. Periods may last longer than usual and require changing pads or tampons more often.
Some women notice their periods become much heavier than normal. Bleeding that soaks through a pad or tampon every hour for several hours needs medical care.
Excessive bleeding during periods can include large clots or bleeding between periods. This type of bleeding can lead to anemia and more fatigue.
Potential Complications Associated With Low Platelets
Low platelet counts can lead to serious bleeding problems that affect multiple body systems. The most dangerous complications include uncontrolled bleeding, internal hemorrhage, and organ-related issues that require immediate medical attention.
Risk of Excessive or Prolonged Bleeding
People with low platelets experience bleeding that lasts much longer than normal. Small cuts or injuries that would typically stop bleeding within minutes can continue for hours.
Nosebleeds become frequent and difficult to control. Many patients notice they bleed heavily after dental work or minor procedures.
Common bleeding sites include:
- Gums during brushing or flossing
- Nose without any injury
- Small cuts from shaving
- Menstrual periods that are heavier than usual
Bruising appears easily from minor bumps or pressure. These bruises often look larger and darker than normal bruises.
The bleeding happens because platelets help form clots. When platelet counts drop below 50,000 per microliter, prolonged bleeding becomes more common[2].
Internal Bleeding and Hemorrhage
Internal bleeding represents the most serious complication of low platelets. This type of bleeding occurs inside the body where it cannot be seen or easily detected.
Severe thrombocytopenia increases the risk of internal bleeding[2] in critical areas. The digestive system often bleeds first, causing black or bloody stools.
Warning signs of internal hemorrhage:
- Blood in urine (pink, red, or dark colored)
- Vomit that looks like coffee grounds
- Severe headaches with confusion
- Weakness and dizziness
Brain bleeding is the most dangerous type of internal hemorrhage. This life-threatening condition can cause permanent damage or death.
Patients with platelet counts below 20,000 face the highest risk for spontaneous internal bleeding.
Impact on Immune System
Low platelets can weaken the body’s ability to fight infections. Platelets contain proteins that help the immune system respond to bacteria and viruses.
When platelet counts drop, wounds heal more slowly. Open cuts and injuries stay vulnerable to infection for longer periods.
The immune system works harder to compensate for missing platelets. This extra work can make patients feel tired and weak.
Some medications used to treat low platelets can further suppress immune function. Patients may need extra precautions to avoid getting sick.
Immune system effects include:
- Slower wound healing
- Higher infection risk at injury sites
- Increased fatigue
- Reduced ability to fight common illnesses
Enlarged Spleen and Splenomegaly
The spleen often grows larger when trying to filter damaged platelets from the blood. This condition, called splenomegaly, creates additional problems for patients.
An enlarged spleen can trap and destroy even more platelets. This creates a cycle where platelet counts continue to drop.
Patients with splenomegaly may feel fullness or pain in the upper left side of their belly. The enlarged organ can press against other structures.
Signs of an enlarged spleen:
- Left side abdominal pain
- Feeling full after eating small amounts
- Pain that spreads to the left shoulder
- Visible swelling in the upper abdomen
Doctors can feel an enlarged spleen during physical exams. Blood tests and imaging help confirm the diagnosis and monitor the condition.
Common Causes of Low Platelet Count
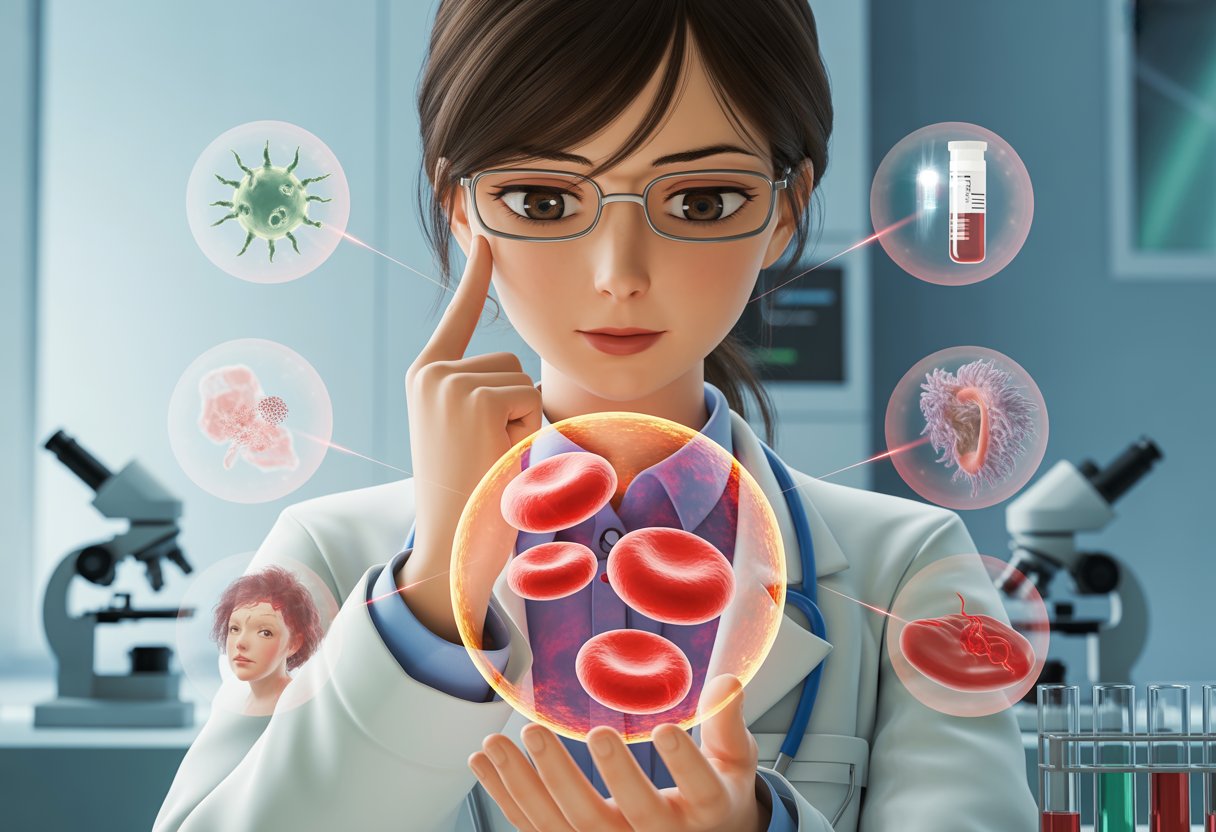
Low platelet counts happen when the body makes too few platelets, destroys too many platelets, or traps platelets in an enlarged spleen. Each of these problems has different causes that range from infections and medications to serious diseases like cancer.
Reduced Platelet Production
The bone marrow makes platelets along with other blood cells. When bone marrow doesn’t work properly, platelet counts drop.
Blood cancers are a major cause of low platelet production. Leukemia and lymphoma can crowd out normal blood cells in the bone marrow. These cancers prevent the bone marrow from making enough healthy platelets.
Aplastic anemia happens when bone marrow stops making enough blood cells, including platelets. This rare condition can be caused by viral infections, certain medications, or exposure to toxic chemicals.
Cancer treatments often reduce platelet production. Chemotherapy and radiation therapy target fast-growing cells, which includes the cells that make platelets in bone marrow.
Viral infections can temporarily lower platelet production. Hepatitis C and HIV are common viral causes of low platelets. These infections can affect bone marrow function for weeks or months.
Myelodysplastic syndrome causes bone marrow to make abnormal blood cells. This condition mostly affects older adults and can lead to very low platelet counts.
Alcohol abuse damages bone marrow over time. Heavy drinking reduces the body’s ability to make platelets and other blood cells.
Increased Platelet Destruction
Sometimes the body destroys platelets faster than it makes them. This often happens when the immune system attacks platelets by mistake.
Immune thrombocytopenia (also called idiopathic thrombocytopenic purpura or ITP) is the most common autoimmune cause. The immune system creates antibodies that destroy platelets. This condition can happen suddenly or develop slowly over time.
Other autoimmune conditions also cause platelet destruction. Lupus and rheumatoid arthritis can trigger the immune system to attack platelets along with other body tissues.
Drug-induced thrombocytopenia happens when medications cause platelet destruction. Heparin is a well-known cause through a condition called heparin-induced thrombocytopenia (HIT). Other medications like certain antibiotics and heart drugs can also cause this problem.
Bacterial infections can lead to platelet destruction through several mechanisms. Severe infections may cause the immune system to destroy platelets or use up platelets faster than normal.
Pregnancy sometimes causes mild platelet destruction. Gestational thrombocytopenia affects about 5% of pregnant women and usually resolves after delivery.
Platelet Sequestration in the Spleen
The spleen normally filters old platelets from the blood. When the spleen gets too big, it traps too many platelets and causes low counts in the bloodstream.
Splenomegaly (enlarged spleen) is often caused by liver disease. Cirrhosis from alcohol abuse, hepatitis, or other liver conditions can cause the spleen to grow larger. An enlarged spleen can trap up to 90% of platelets instead of the normal 30%.
Liver disease causes low platelets through multiple pathways. Besides causing splenomegaly, severe liver problems can reduce platelet production[2] and increase platelet destruction.
Blood pooling in an enlarged spleen reduces the number of platelets available in circulation. Even though the body has enough total platelets, most stay trapped in the spleen rather than flowing through blood vessels.
Portal hypertension from liver disease increases pressure in blood vessels connected to the spleen. This higher pressure makes the spleen enlarge and trap more platelets than normal.
Types of Thrombocytopenia and Related Disorders
Low platelet counts can develop through different mechanisms, with some disorders causing the immune system to attack platelets while others involve blood clotting problems or medication reactions. Each type has distinct causes, symptoms, and treatment approaches.
Immune Thrombocytopenic Purpura (ITP)
Immune thrombocytopenic purpura, also called idiopathic thrombocytopenic purpura or immune thrombocytopenia, occurs when the body’s immune system mistakenly attacks and destroys its own platelets. This autoimmune condition can affect both children and adults.
ITP appears in two main forms:
- Acute ITP: Develops suddenly, most common in children after viral infections
- Chronic ITP: Develops gradually and lasts longer than 12 months, more common in adults
Patients with ITP typically experience easy bruising, purple spots on the skin called petechiae, and bleeding from the gums or nose. Women may have unusually heavy menstrual periods.
The exact cause remains unknown in many cases. However, certain infections, medications, or other autoimmune disorders can trigger the condition.
Treatment options include corticosteroids, immune globulin therapy, and medications that help increase platelet production. In severe cases, doctors may recommend spleen removal.
Thrombotic Thrombocytopenic Purpura (TTP)
Thrombotic thrombocytopenic purpura (TTP) is a rare but serious blood disorder where small blood clots form throughout the body’s small blood vessels. These clots use up platelets, causing dangerously low platelet counts.
TTP creates five main symptoms known as the classic pentad:
- Low platelet count
- Destruction of red blood cells
- Neurological problems
- Kidney dysfunction
- Fever
The condition occurs when an enzyme called ADAMTS13 doesn’t work properly or is missing entirely. This enzyme normally breaks down large blood clotting proteins.
TTP can be inherited or acquired later in life. Acquired TTP often develops when the immune system produces antibodies against the ADAMTS13 enzyme.
Without treatment, TTP can be fatal within weeks. Emergency treatment involves plasma exchange therapy, which removes the patient’s plasma and replaces it with donor plasma containing the missing enzyme.
Disseminated Intravascular Coagulation (DIC)
Disseminated intravascular coagulation occurs when the body’s normal blood clotting process becomes overactive throughout the circulatory system. This widespread clotting uses up platelets and clotting factors, leading to both excessive clotting and severe bleeding.
DIC always develops as a complication of another serious medical condition. Common triggers include:
- Severe infections (sepsis)
- Major trauma or burns
- Certain cancers
- Complications during childbirth
- Snake bites
Patients experience a paradoxical combination of blood clots in small vessels and uncontrolled bleeding from various sites. Symptoms include bruising, bleeding from wounds that won’t stop, and organ dysfunction.
Laboratory tests show low platelet counts, decreased clotting factors, and elevated markers of clot breakdown. Treatment focuses on addressing the underlying cause while providing supportive care with blood products and clotting factors as needed.
Heparin-Induced Thrombocytopenia
Heparin-induced thrombocytopenia (HIT) is a serious reaction to heparin, a blood-thinning medication commonly used in hospitals. Despite causing low platelet counts, HIT paradoxically increases the risk of dangerous blood clots.
HIT develops when the immune system creates antibodies against complexes formed between heparin and a protein called platelet factor 4. These antibodies activate platelets, causing both platelet consumption and clot formation.
Two types of drug-induced thrombocytopenia related to heparin exist:
- Type I: Mild, non-immune reaction that resolves quickly
- Type II: Severe, immune-mediated reaction (true HIT)
HIT typically develops 5-10 days after starting heparin therapy. Platelet counts usually drop by 50% or more from baseline levels.
The condition requires immediate discontinuation of all heparin products and switching to alternative blood thinners. Patients need monitoring for blood clots even after stopping heparin, as the risk can persist for several weeks.
Diagnosing Low Platelet Count
Doctors use blood tests, physical exams, and medical history to find low platelet counts. Additional tests may check bone marrow or rule out other conditions.
Physical Examination and Medical History
Doctors start by checking for signs of bleeding or bruising on the skin. They look for small red spots called petechiae and larger purple bruises.
The physical exam includes checking the spleen size. An enlarged spleen can trap platelets and cause low counts.
Medical history helps doctors find possible causes. They ask about:
- Current medications
- Recent infections
- Family history of bleeding problems
- Previous blood disorders
Key symptoms doctors look for:
- Easy bruising
- Frequent nosebleeds
- Heavy menstrual periods
- Bleeding gums
The exam also checks lymph nodes for swelling. This can point to blood cancers or immune problems that affect platelets.
Laboratory Blood Tests
A complete blood count (CBC)[2] is the main test for checking platelet levels. Normal platelet counts range from 150,000 to 450,000 per microliter of blood.
The CBC shows if other blood cells are also low. This helps doctors find the cause of thrombocytopenia.
A blood smear lets doctors look at platelets under a microscope. They check the size and shape of platelets and other blood cells.
Platelet count levels:
- Normal: 150,000-450,000 per microliter
- Mild low: 101,000-140,000 per microliter
- Moderate low: 51,000-100,000 per microliter
- Severe low: 21,000-50,000 per microliter
Additional blood tests may check for antibodies. These can destroy platelets in autoimmune conditions.
Further Diagnostic Procedures
Hematologists may order a bone marrow test if the cause remains unclear. This procedure checks if the bone marrow makes enough platelets.
The bone marrow biopsy involves taking a small sample from the hip bone. It shows whether platelet production is normal or reduced.
Doctors may test for specific conditions like immune thrombocytopenic purpura (ITP). This requires ruling out other causes first.
Advanced tests include:
- Bone marrow aspiration
- Platelet antibody tests
- Genetic testing
- Imaging scans of the spleen
Some patients need repeat blood tests to track platelet levels over time. This helps determine if the condition is getting worse or better.
Hematologists coordinate care when platelet counts are very low or the cause is complex.
Treatment and Management of Thrombocytopenia
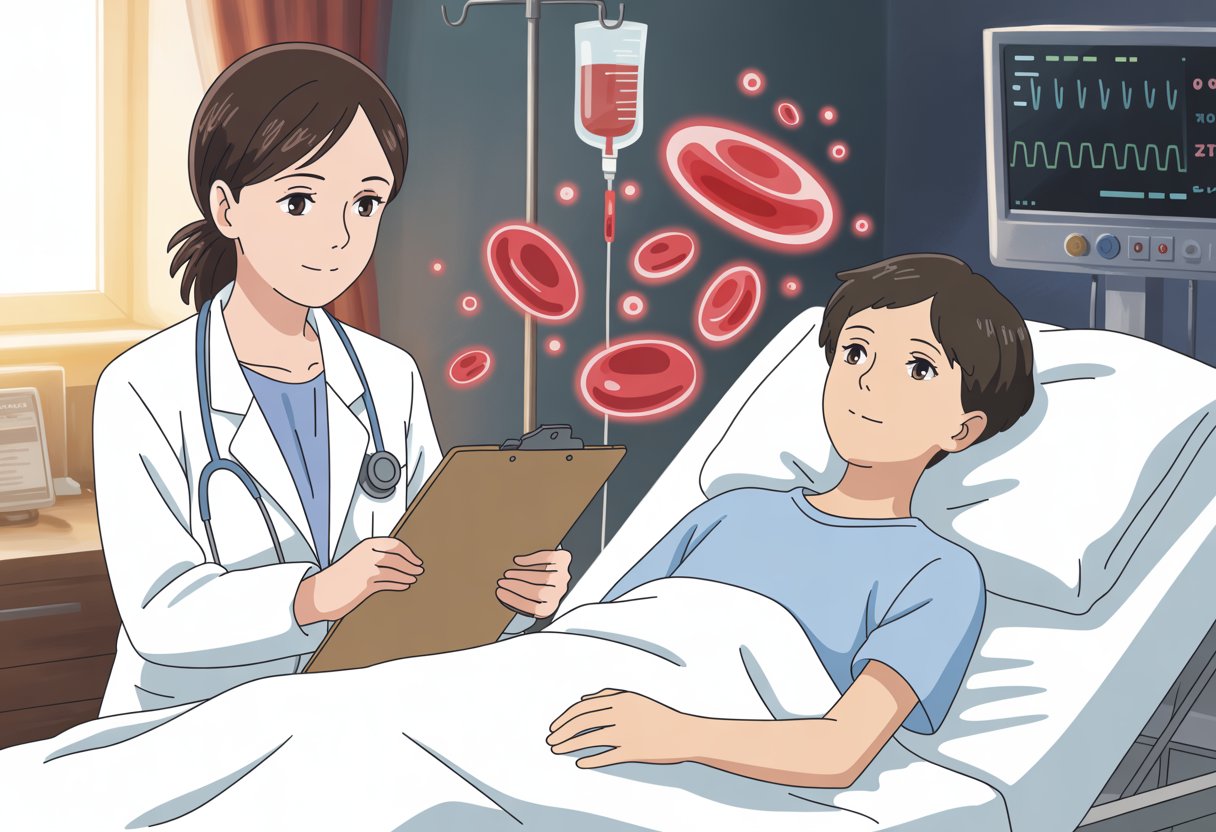
Treatment for thrombocytopenia[3] focuses on raising platelet counts to safe levels while addressing the root cause. The approach varies based on how severe the condition is and what caused it.
Addressing Underlying Causes
Doctors first identify and treat the condition causing low platelets. This step is crucial for long-term success.
Drug-induced thrombocytopenia requires stopping the problem medication immediately. Common drugs that cause low platelets include quinine, some antibiotics, and certain heart medications. Most patients see their platelet counts improve within 7-10 days after stopping the drug.
Autoimmune conditions need specific treatments to control the immune system. Doctors may treat infections like H. pylori bacteria, which can trigger platelet destruction.
Liver disease patients need treatment for their underlying condition. This might include managing hepatitis or reducing alcohol consumption.
Cancer patients often develop low platelets from chemotherapy. Doctors may adjust treatment schedules or doses to help platelet counts recover.
Medical Treatments and Medications
Several medications can increase platelet production or reduce platelet destruction.
Corticosteroids like prednisone are often the first treatment. These drugs reduce immune system activity and help stop platelet destruction. Most patients start seeing results within days to weeks.
Thrombopoietin receptor agonists help the bone marrow make more platelets. Eltrombopag is taken by mouth daily. Romiplostim requires weekly injections under the skin.
Rituximab targets specific immune cells that destroy platelets. This medication is given through an IV over several weeks.
Plasma exchange removes harmful antibodies from the blood. This treatment is used for severe cases or specific conditions like TTP.
Splenectomy (spleen removal) may be needed when other treatments fail. The spleen often destroys platelets, so removing it can help counts stay higher.
Platelet Transfusions
Platelet transfusions provide immediate but temporary help when counts are dangerously low.
Doctors recommend platelet transfusions[4] when patients have active bleeding or platelet counts below 10,000. Patients also need transfusions before surgery or procedures.
The transfusion process takes 1-2 hours through an IV. Platelets from donors only last 3-5 days in the body.
Blood transfusions may also be needed if patients have lost significant blood. These provide red blood cells rather than platelets.
Patients may need multiple transfusions depending on their condition. Some people develop antibodies that make future transfusions less effective.
Lifestyle Adjustments and Preventive Measures
Patients with low platelets must take steps to prevent bleeding and injury.
Activity restrictions are important for safety. Patients should avoid contact sports[4] and activities with high injury risk when platelet counts are below 50,000.
Medication changes help reduce bleeding risk. Patients must avoid NSAIDs like ibuprofen and aspirin. These drugs interfere with platelet function and increase bleeding.
Injury prevention includes using soft toothbrushes and electric razors. Patients should wear protective gear when needed and avoid sharp objects.
Bleeding awareness helps patients recognize problems early. They should watch for unusual bruising, nosebleeds, or blood in urine or stool.
Regular blood tests monitor platelet levels and treatment progress. Patients work closely with their healthcare team to adjust treatments as needed.
Frequently Asked Questions
Low platelet counts raise many concerns about symptoms, treatment options, and potential health risks. Understanding the warning signs, dietary approaches, and when to seek medical care helps people make informed decisions about their health.
What are the common symptoms associated with a decrease in platelets?
People with low platelet counts often experience easy bruising and excessive bleeding. Small cuts may bleed longer than normal, and bruises appear with minimal bumps or injuries.
Bleeding gums during tooth brushing is another common sign. Nosebleeds may happen more often and last longer than usual.
Heavy menstrual periods affect women with thrombocytopenia. Signs of a low platelet count[1] can also include tiny red or purple spots on the skin called petechiae.
Blood in urine or stool indicates more serious bleeding. Severe cases may cause internal bleeding that requires immediate medical attention.
What dietary or lifestyle changes can help increase platelet count?
Foods rich in folate support platelet production in the bone marrow. Leafy green vegetables, beans, and fortified cereals provide good folate sources.
Vitamin B12 helps maintain healthy blood cell levels. Fish, meat, dairy products, and fortified foods contain this important vitamin.
Iron-rich foods like red meat, spinach, and lentils support overall blood health. Vitamin C from citrus fruits helps the body absorb iron better.
Avoiding alcohol protects the bone marrow and prevents further platelet damage. Regular exercise improves overall blood circulation and health.
Getting enough sleep allows the body to produce blood cells more effectively. Avoiding medications that thin the blood also helps prevent excessive bleeding.
At what platelet level should an individual be concerned about their health?
Normal platelet counts range from 150,000 to 450,000 per microliter of blood. Mild thrombocytopenia occurs with platelet levels between 101,000 and 140,000[2].
Moderate thrombocytopenia involves platelet counts between 51,000 and 100,000 per microliter. This level often requires medical monitoring and may cause noticeable bleeding symptoms.
Severe thrombocytopenia occurs when platelet counts drop between 21,000 and 51,000 per microliter. This level carries serious bleeding risks and requires immediate medical care.
Platelet counts below 20,000 per microliter create life-threatening bleeding risks. Emergency treatment becomes necessary at these extremely low levels.
Are there any rapid methods to elevate platelet counts that are effective?
Platelet transfusions provide the fastest way to raise platelet counts in emergency situations. Doctors use this treatment when bleeding risks become life-threatening.
Corticosteroid medications like prednisone can increase platelet production within days to weeks. These drugs work by reducing immune system attacks on platelets.
Intravenous immunoglobulin (IVIG) therapy helps raise platelet counts quickly in some cases. This treatment blocks antibodies that destroy platelets.
Medications that stimulate platelet production take several weeks to show effects. These drugs work slower than transfusions but provide longer-lasting results.
Emergency treatments focus on stopping active bleeding rather than slowly building platelet counts. Quick interventions save lives when severe bleeding occurs.
Can a low platelet count be indicative of cancer or other serious health conditions?
Blood cancers like leukemia or lymphoma can cause low platelet counts[2] by affecting bone marrow function. These cancers prevent normal platelet production.
Autoimmune diseases cause the immune system to destroy healthy platelets. Conditions like lupus and rheumatoid arthritis commonly affect platelet levels.
Liver disease reduces platelet production and increases destruction. The spleen may become enlarged and trap more platelets than normal.
Viral infections temporarily lower platelet counts in many cases. Most viral-related drops resolve as the infection clears.
Certain medications destroy platelets as a side effect. Blood thinners, some antibiotics, and chemotherapy drugs commonly cause this problem.
What underlying issues can lead to a reduction in platelet levels?
Bone marrow disorders prevent adequate platelet production[5]. Conditions like aplastic anemia and myelodysplastic syndrome affect blood cell creation.
Immune system problems cause antibodies to attack and destroy platelets. Immune thrombocytopenic purpura (ITP) specifically targets platelets for destruction.
Enlarged spleen traps and destroys too many platelets. Liver disease, infections, and blood cancers commonly cause spleen enlargement.
Pregnancy naturally lowers platelet counts in about 5% of women. These levels usually return to normal after delivery.
Nutritional deficiencies in vitamin B12, folate, or iron impair platelet production. Poor diet or absorption problems create these deficiencies over time.
References
- thrombocytopenia, occurs when blood has too few platelets. https://www.verywellhealth.com/living-with-low-platelets-what-you-need-to-know-2252431 Accessed November 3, 2025
- Thrombocytopenia: Symptoms, Stages & Treatment. https://my.clevelandclinic.org/health/diseases/14430-thrombocytopenia Accessed November 3, 2025
- What are the treatment options for thrombocytopenia (low platelet count)?. https://www.droracle.ai/articles/101929/treatment-of-thrombocytopenias- Accessed November 3, 2025
- Thrombocytopenia: Evaluation and Management. https://www.aafp.org/pubs/afp/issues/2022/0900/thrombocytopenia.html Accessed November 3, 2025
- Overview of Thrombocytopenia - Blood Disorders. https://www.merckmanuals.com/home/blood-disorders/platelet-disorders/overview-of-thrombocytopenia Accessed November 3, 2025
