SNA-based therapies represent a groundbreaking approach to medicine that combines DNA or RNA with tiny nanoparticles to create more effective treatments. These spherical nucleic acid structures wrap medications in genetic material, allowing drugs to enter cells more easily and target specific diseases with greater precision than traditional treatments. Scientists have discovered that this technology can transform poorly performing drugs into powerful, targeted therapies.

The potential applications for SNA-based treatments extend far beyond cancer care. Researchers are exploring how these DNA-wrapped nanostructures could revolutionize treatments for infectious diseases, brain disorders, and autoimmune conditions. The technology works by taking advantage of natural cell receptors that recognize and pull these structures inside, delivering medication exactly where it needs to go.
Currently, seven SNA-based therapies are in clinical trials[1], marking a significant step toward bringing this technology to patients. Early animal studies have shown remarkable results, with some treatments proving thousands of times more effective than standard medications while causing fewer side effects.
Key Takeaways
- SNA-based therapies use DNA-wrapped nanoparticles to deliver drugs more effectively into target cells
- These treatments show promise for cancer, infectious diseases, neurological disorders, and autoimmune conditions
- Seven SNA therapies are currently being tested in human clinical trials with encouraging early results
Understanding SNA-Based Therapies
Spherical nucleic acids represent emerging amplifiers for therapeutic nanoplatforms[2] that differ significantly from traditional gene delivery methods. These three-dimensional structures offer enhanced cellular uptake and improved stability compared to linear nucleic acids.
What Are Spherical Nucleic Acids (SNAs)?
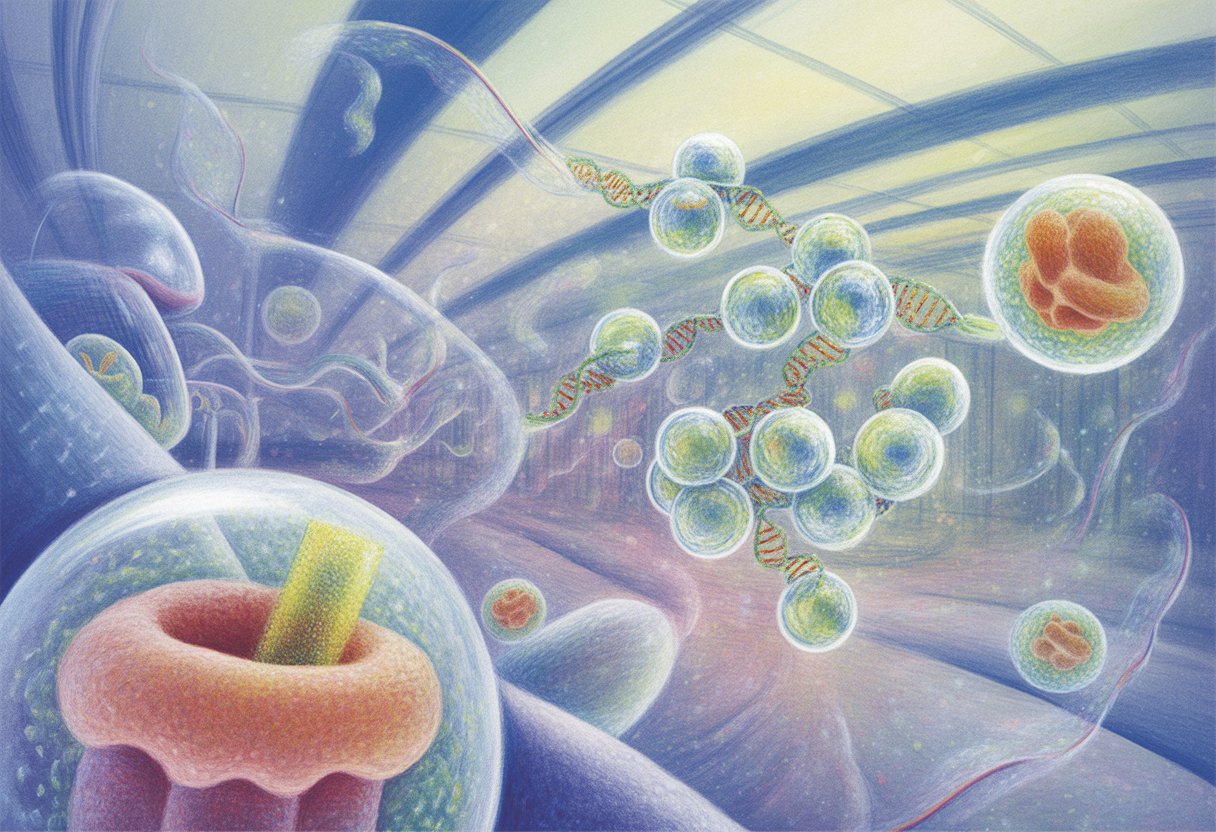
Spherical nucleic acids are three-dimensional nanostructures composed of nucleic acids arranged around a central core. The core can be made from various materials including gold nanoparticles, liposomes, or proteins.
Key structural features include:
- Dense nucleic acid shell surrounding the core
- Radial orientation of DNA or RNA strands
- Typically 10-100 nanometers in diameter
SNAs possess unique physicochemical properties that distinguish them from free nucleic acids. They demonstrate increased resistance to nuclease degradation. The spherical arrangement provides multiple binding sites for cellular receptors.
These structures can carry different types of nucleic acids simultaneously. They maintain their three-dimensional shape in biological environments. The dense packing of nucleic acids creates a highly charged surface.
Structural Nanomedicine vs. Traditional Nanomedicine
Traditional nanomedicine relies on encapsulation or attachment of therapeutic agents to carrier particles. Drugs are typically loaded inside or onto the surface of delivery vehicles like liposomes or polymeric nanoparticles.
Structural nanomedicine takes a different approach. The therapeutic agent becomes part of the nanostructure itself. SNAs exemplify this concept by making nucleic acids the primary structural component.
Traditional approach limitations:
- Drug leakage during transport
- Burst release effects
- Limited loading capacity
- Carrier toxicity concerns
Structural nanomedicine advantages:
- Therapeutic agent is integral to structure
- Controlled release through structural changes
- Higher drug-to-carrier ratios
- Reduced carrier-related side effects
This structural integration eliminates the need for separate packaging steps. It also provides better control over drug release kinetics.
Mechanism of Action in the Body
SNAs enter cells through enhanced cellular uptake mechanisms. Their spherical structure and high surface charge facilitate binding to cell membranes. They can cross cellular barriers more effectively than linear nucleic acids.
SNA nanoparticle conjugates demonstrate the ability to enter multiple cell types and penetrate both tumor and normal tissue[3]. Once inside cells, they release their nucleic acid payload through enzymatic degradation or structural changes.
The mechanism involves several steps:
- Cellular binding – SNAs attach to membrane receptors
- Internalization – Cells engulf the structures through endocytosis
- Intracellular release – Nucleic acids are freed from the core
- Target engagement – Released nucleic acids interact with their targets
SNAs can neutralize target gene expression effectively. They trigger downstream cellular responses like apoptosis in cancer cells. The spherical structure protects the nucleic acids from degradation during transport.
SNA-Based Therapies in Cancer Treatment
SNAs offer a targeted approach to cancer treatment by entering cancer cells more efficiently than traditional drugs while reducing harmful effects on healthy tissue. Recent studies show these treatments can be thousands of times more effective than standard chemotherapy.
Targeting Cancer Cells With SNAs
SNAs use a unique targeting system that takes advantage of cell surface receptors. Cancer cells, particularly myeloid cells, have high levels of scavenger receptors on their surfaces.
These receptors recognize SNAs and pull them into the cell naturally. This process eliminates the need to force drugs through cell walls.
Key targeting advantages:
- Cells invite SNAs inside automatically
- No forced entry required
- Higher uptake in cancer cells with more receptors
Once inside the cancer cell, enzymes break down the DNA shell surrounding the SNA. This releases the chemotherapy drug directly where it needs to work.
The SNA-based treatment entered cancer cells 12.5 times more efficiently[4] than the standard drug in recent tests. This improved delivery means more drug reaches the cancer cells that need to be destroyed.
The targeting system works especially well for blood cancers like acute myeloid leukemia. These cancer cells have even more scavenger receptors than other cell types.
Efficacy Compared to Conventional Chemotherapy
SNA-based cancer treatments show dramatic improvements over traditional chemotherapy drugs. The most striking results come from tests using the common chemotherapy drug 5-fluorouracil.
Researchers redesigned this drug as an SNA structure. The results were remarkable compared to the original drug.
Effectiveness improvements:
- 20,000 times more effective at killing cancer cells
- 59 times better at slowing cancer progression
- 12.5 times better cell entry rate
In mouse studies with acute myeloid leukemia, the new drug kills cancer 20,000x more effectively[5] than the original version. The treatment eliminated leukemia cells almost completely from blood and spleen tissue.
The improved performance comes from better drug solubility. Traditional chemotherapy drugs often dissolve poorly in body fluids. Less than 1% of some drugs actually dissolve properly.
SNAs solve this problem by incorporating the drug into their DNA structure. This makes the entire treatment water-soluble and easier for the body to use.
Reduction of Side Effects
Traditional chemotherapy drugs damage both cancer cells and healthy cells. This causes serious side effects like nausea, fatigue, and sometimes heart problems.
SNA-based treatments target cancer cells specifically. Healthy tissues remain largely unharmed during treatment.
Side effect improvements:
- No detectable side effects in animal tests
- Healthy cells stay protected
- Focused drug delivery reduces whole-body exposure
The selective targeting means doctors can use higher drug doses where needed. Instead of flooding the entire body with chemotherapy, SNAs deliver concentrated treatment to cancer cells only.
Patients may experience fewer treatment interruptions due to side effects. This could lead to better treatment outcomes and improved quality of life during cancer therapy.
Current animal studies show promising safety results. Researchers found no noticeable side effects even with the highly effective SNA treatments.
Applications in Acute Myeloid Leukemia (AML)
SNA-based therapies offer targeted approaches for treating acute myeloid leukemia by directly interfering with cancer cell gene expression and providing selective delivery to malignant cells. These treatments work by silencing specific genes that drive AML progression while minimizing damage to healthy blood cells.
How SNAs Treat AML
SNAs target specific genes that fuel acute myeloid leukemia growth and survival. They work by binding to messenger RNA sequences that produce proteins essential for leukemia cell function.
Key therapeutic targets include:
- BCL-2 family proteins that prevent cancer cell death
- FLT3 mutations found in 30% of AML patients
- MYC oncogenes that drive rapid cell division
The SNAs enter leukemia cells and attach to their target RNA molecules. This stops the cells from making proteins they need to survive and multiply.
Clinical studies show SNAs can reduce leukemia cell counts in bone marrow samples. They work especially well against AML cells that resist traditional chemotherapy drugs.
Some SNAs target multiple genes at once. This approach helps prevent cancer cells from developing resistance to treatment.
Delivery and Selectivity for Leukemia Cells
SNAs use specialized delivery systems to reach acute myeloid leukemia cells while avoiding healthy tissue. The most common approach involves nanoparticle carriers that recognize specific markers on AML cells.
Delivery mechanisms include:
- Lipid nanoparticles that fuse with cell membranes
- Antibody-conjugated carriers that bind to leukemia antigens
- Direct cellular uptake through endocytosis
Leukemia cells often express higher levels of certain surface proteins compared to normal blood cells. SNAs can be designed to target these unique markers.
The selectivity reduces side effects that plague traditional chemotherapy. Normal bone marrow cells receive less exposure to the therapeutic agents.
Recent advances in AML targeted therapy[6] show promise for improving delivery precision. Researchers continue developing better ways to ensure SNAs reach their intended targets.
Biological Pathways and Target Locations
SNA-based therapies follow specific pathways once they enter the body, with blood and spleen serving as primary distribution sites. These therapies use specialized mechanisms to enter cells and reach their intended targets.
Uptake by Blood and Spleen
When SNA therapies enter the bloodstream, they distribute rapidly throughout the circulatory system. The blood acts as the main highway for these treatments to reach different organs and tissues.
The spleen plays a critical role in processing SNA therapies. This organ contains many immune cells that can capture and process these treatments. The spleen’s structure allows it to filter blood effectively.
Key distribution patterns include:
- Immediate blood circulation within minutes
- Spleen accumulation within 1-2 hours
- Gradual tissue distribution over several hours
The liver also receives significant amounts of SNA therapies from the blood. Kidney filtration can affect how long these treatments stay in the body. Some SNA therapies are designed to target specific tissues by using special coating molecules.
Cellular Entry Mechanisms
SNA therapies enter cells through several different pathways. The most common method involves the cell membrane wrapping around the therapy particles. This process is called endocytosis.
Receptor-mediated endocytosis occurs when SNA therapies bind to specific proteins on cell surfaces. These proteins act like doorways that allow the therapies to enter. Different cell types have different receptors available.
Main entry mechanisms:
- Clathrin-mediated endocytosis
- Caveolin-dependent uptake
- Micropinocytosis
- Direct membrane fusion
Once inside cells, SNA therapies must escape from cellular compartments to reach their targets. They often need to break free from endosomes before these compartments fuse with lysosomes. The timing of this escape is crucial for treatment success.
Progress in Clinical Trials
SNA-based therapies have shown promising results in early clinical testing, with trials demonstrating safety and brain penetration capabilities. The field faces significant translational hurdles but continues advancing toward broader therapeutic applications.
Current Status of SNA-Based Therapies
Early phase clinical trials have established important safety profiles for SNA therapeutics. Clinical trials in glioblastoma and solid tumors[7] have demonstrated that these therapies can safely cross the blood-brain barrier.
Two key trials have advanced the field significantly. NCT03020017[8] tested gene-regulatory siRNA-based SNAs in glioblastoma patients. NCT03086278[9] evaluated immunostimulatory SNAs carrying CpG-rich oligonucleotides in solid tumor patients.
Both studies confirmed that SNAs represent a safe treatment option. The trials showed these therapies can effectively penetrate brain tissue. This breakthrough addresses one of the biggest challenges in treating brain cancers.
The glioblastoma trial focused on inhibiting oncogene expression. Results showed the therapy could reach tumor sites in the brain. The solid tumor trial tested immune system activation through Toll-like receptor 9 stimulation.
Translational Challenges and Opportunities
Moving SNAs from laboratory to clinical use presents several obstacles. Manufacturing consistent batches of these complex nanoparticles requires precise control. Regulatory agencies need clear guidelines for evaluating these novel therapies.
Delivery remains a critical challenge despite recent progress. While brain penetration has been achieved, targeting specific tissues efficiently needs improvement. Cost-effectiveness must be demonstrated for widespread adoption.
The field benefits from recent advances in nucleic acid therapeutics[10]. These developments provide frameworks for SNA development. Established delivery methods like lipid nanoparticles offer proven pathways.
Opportunities exist in personalized medicine applications. SNAs can be designed for specific genetic targets. This precision approach may lead to more effective treatments with fewer side effects.
Future Directions in Nanomedicine
Scientists are exploring ways to expand SNA-based therapies beyond cancer treatment. These tiny medicines show promise for treating autoimmune conditions and many other diseases that currently have limited treatment options.
Potential Beyond Cancer
Researchers are testing structural nanomedicine approaches[11] for infectious diseases and brain disorders like Alzheimer’s. The precise control over medicine structure could help drugs reach parts of the body that are hard to treat.
Neurological conditions present unique challenges. The brain has protective barriers that block most medicines from entering. SNA-based therapies might be able to cross these barriers more easily.
Infectious diseases could benefit from targeted nanomedicines. These treatments could deliver antibiotics directly to infected cells while avoiding healthy tissue.
Scientists plan to use artificial intelligence to design better nanomedicines. AI can help researchers sort through thousands of possible designs to find the best ones for testing.
The technology behind chemoflares could work for other diseases too. These smart medicines only activate when they find specific disease signals in the body.
Autoimmune Diseases and Other Indications
Autoimmune diseases happen when the immune system attacks healthy body parts. SNA-based therapies could help retrain the immune system to stop these harmful attacks.
Multiple sclerosis and rheumatoid arthritis are two conditions that researchers want to target. These diseases cause inflammation that damages organs and joints over time.
The medicines could deliver instructions to immune cells. These instructions would teach the cells to recognize the difference between healthy tissue and real threats.
Type 1 diabetes might also respond to this approach. The disease destroys cells that make insulin in the pancreas. Nanomedicines could protect these cells from immune system attacks.
Early research shows these therapies can reduce inflammation in lab studies. The next step is testing them in people with autoimmune conditions.
Considerations and Limitations
While SNA-based therapies show promise, researchers face significant hurdles in proving their long-term safety and gaining regulatory approval. The newness of this technology creates uncertainty about extended treatment effects and slows the path to clinical use.
Long-Term Safety and Efficacy
Current clinical data for SNA therapies spans only short time periods. Most studies track patients for months rather than years. This limited timeframe makes it difficult to identify delayed side effects or complications.
The gold nanoparticles used in many SNA designs raise questions about accumulation in organs over time. Scientists need more research to understand how the body processes and eliminates these materials after repeated treatments.
Key safety concerns include:
- Potential immune system reactions to repeated doses
- Unknown effects of long-term nanoparticle exposure
- Limited data on drug interactions
- Unclear impacts on pregnancy and development
Efficacy data remains preliminary for most SNA applications. While RNA interference-based SNA platforms show promise for treating brain tumors[3], larger clinical trials are needed. Many studies involve small patient groups or animal models rather than comprehensive human trials.
Regulatory and Adoption Issues
The FDA treats SNA therapies as novel drug-device combinations. This classification creates complex approval pathways that differ from traditional medications. Companies must demonstrate both the safety of the nanoparticle carrier and the therapeutic nucleic acid payload.
Manufacturing consistency poses another regulatory challenge. Each SNA particle must contain the same number of nucleic acid strands in the same orientation. Small variations in production can affect treatment outcomes.
Regulatory barriers include:
- No established guidelines specific to SNA therapies
- Required toxicology studies for nanoparticle components
- Quality control standards for complex manufacturing processes
- High costs for clinical trial requirements
Healthcare systems face adoption challenges even after approval. SNA therapies require specialized storage conditions and trained personnel for administration. Many hospitals lack the infrastructure needed for these advanced treatments.
Insurance coverage remains uncertain for most SNA-based therapies. The high development costs often translate to expensive treatments that payers may resist covering without strong evidence of cost-effectiveness.
Frequently Asked Questions

SNA-based therapies use unique three-dimensional structures to deliver genetic material directly into cells. These treatments show promise for cancer, skin conditions, and neurological diseases through improved cellular uptake and reduced immune reactions.
How do SNA-based therapies work in treating diseases?
SNA-based therapies work by delivering therapeutic nucleic acids directly into target cells. The spherical structure allows the genetic material to cross cell membranes without needing additional delivery vehicles.
Once inside cells, the nucleic acids can silence harmful genes or replace missing proteins. This process helps treat diseases at their genetic source rather than just managing symptoms.
The three-dimensional design protects the therapeutic material from breaking down in the body. This protection helps the treatment reach its target more effectively than traditional methods.
What types of conditions can be treated with SNA-based therapies?
Cancer represents the primary target for SNA-based therapies. These treatments can deliver drugs directly to tumor cells while avoiding healthy tissue damage.
Skin conditions like psoriasis and eczema respond well to topical SNA applications. The spherical structure penetrates skin barriers more easily than conventional treatments.
Neurological diseases including Alzheimer’s and Parkinson’s show potential for SNA therapy. The treatments can cross the blood-brain barrier to reach affected brain cells.
Autoimmune disorders may benefit from SNA therapies that can modify immune system responses. Eye diseases also represent promising treatment areas due to improved drug delivery to ocular tissues.
Are there any completed clinical trials on SNA-based therapies, and what do they reveal?
Several Phase I and Phase II clinical trials have tested SNA-based therapies for various conditions. These early studies focus primarily on safety and dosing rather than full effectiveness.
Cancer trials show that SNA therapies can be safely administered with fewer side effects than traditional chemotherapy. Patients tolerated the treatments well across different dose levels.
Skin condition trials demonstrate improved drug penetration and reduced inflammation. The results suggest better outcomes compared to standard topical treatments.
Most completed trials involve small patient groups and short treatment periods. Larger Phase III trials are needed to confirm long-term effectiveness and safety.
What distinguishes spherical nucleic acid (SNA) therapies from traditional nucleic acid-based treatments?
The spherical structure sets SNAs apart from linear nucleic acid treatments. This three-dimensional design improves stability and cellular uptake compared to flat DNA or RNA molecules.
SNAs enter cells through natural uptake processes without needing viral vectors or lipid carriers. Traditional nucleic acid therapies often require these additional delivery systems that can cause immune reactions.
The dense arrangement of nucleic acids on the spherical surface increases treatment potency. Each SNA particle carries multiple therapeutic molecules compared to single-strand treatments.
SNAs resist breakdown by enzymes in the body better than linear nucleic acids. This stability means treatments last longer and work more effectively at lower doses.
What are the potential side effects or risks associated with SNA-based therapies?
Early clinical trials report fewer side effects with SNA therapies compared to traditional treatments. Most patients experience only mild reactions at injection sites.
Common side effects include temporary redness, swelling, or pain where the treatment is given. These reactions typically resolve within a few days without additional treatment.
Some patients may develop immune responses to the spherical structures. However, these reactions appear less severe than those seen with viral delivery systems.
Long-term effects remain unknown since SNA therapies are relatively new. Researchers continue monitoring patients from completed trials to identify any delayed reactions.
How does the delivery mechanism of SNA-based therapies improve cellular uptake?
The spherical shape allows SNAs to interact with cell surface receptors more effectively than linear molecules. Multiple contact points increase the chance of successful cellular entry.
SNAs use the cell’s natural endocytosis process to gain entry. This mechanism avoids the need for membrane disruption or carrier proteins that other therapies require.
The high density of nucleic acids on the surface creates stronger binding to target cells. This improved binding leads to better uptake and higher concentrations inside cells.
Once inside, the spherical structure protects the therapeutic material from cellular enzymes. This protection ensures more of the treatment reaches its intended target within the cell.
References
- Reengineered Drug: More Effective, Less Harmful Chemotherapy. https://www.azonano.com/news.aspx?newsID=41562 Accessed November 6, 2025
- Spherical nucleic acids: emerging amplifiers for therapeutic nanoplatforms. https://pubs.rsc.org/as/content/articlelanding/2024/nr/d3nr05971e Accessed November 6, 2025
- Just a moment.... https://www.science.org/doi/10.1126/scitranslmed.3006839 Accessed November 6, 2025
- Cancer therapy breakthrough: New chemotherapy agent proves 20,000 times more effective and free of side effects in animal trials. https://www.notebookcheck.net/Cancer-therapy-breakthrough-New-chemotherapy-agent-proves-20-000-times-more-effective-and-free-of-side-effects-in-animal-trials.1154948.0.html Accessed November 6, 2025
- Just a moment.... https://scitechdaily.com/new-drug-kills-cancer-20000x-more-effectively-with-no-detectable-side-effects/ Accessed November 6, 2025
- 10 Acute Myeloid Leukemia Medications and Targeted Therapies to Know in 2025. https://int.livhospital.com/10-acute-myeloid-leukemia-medications-and-targeted-therapies-to-know-in-2025/ Accessed November 6, 2025
- Clinical trials in glioblastoma and solid tumors. https://www.hilarispublisher.com/open-access/from-bench-to-bedside-precision-therapeutics-using-spherical-nucleic-acids-for-cancer-treatment.pdf Accessed November 6, 2025
- A first-in-human phase 0 clinical study of RNA interference-based spherical nucleic acids in patients with recurrent glioblastoma. https://pubmed.ncbi.nlm.nih.gov/33692132/ Accessed November 6, 2025
- A first-in-human phase 1 study of cavrotolimod, a TLR9 agonist spherical nucleic acid, in healthy participants: Evidence of immune activation. https://pubmed.ncbi.nlm.nih.gov/36582243/ Accessed November 6, 2025
- Just a moment.... https://www.cell.com/molecular-therapy-family/nucleic-acids/fulltext/S2162-2531(24)00327-5 Accessed November 6, 2025
- Shape Matters for Future of Nano Cancer Treatments. https://scienceblog.com/shape-matters-for-future-of-nano-cancer-treatments/ Accessed November 6, 2025
