When blood tests show high AST levels[1], many people worry about what this means for their health. High AST levels typically indicate damage to tissues where this enzyme is found, most commonly the liver, heart, or muscles, and may require further medical evaluation to determine the underlying cause.

AST, or aspartate aminotransferase, is an enzyme that helps the body process amino acids. Under normal conditions, AST stays inside cells doing its job. When cells become damaged or injured, they release AST into the bloodstream, causing blood levels to rise above the normal range.
Elevated liver enzymes like AST[2] can happen for many different reasons, from temporary issues like medication effects to more serious conditions requiring treatment. Understanding what high AST means and what steps to take next can help people make informed decisions about their health care.
Key Takeaways
- High AST levels usually mean cells in the liver, heart, or muscles have been damaged and released the enzyme into the blood
- Many different conditions can cause elevated AST, ranging from temporary issues to serious diseases that need treatment
- Additional tests are often needed to find the exact cause and determine the best treatment plan
What Is AST and Why Is It Important?
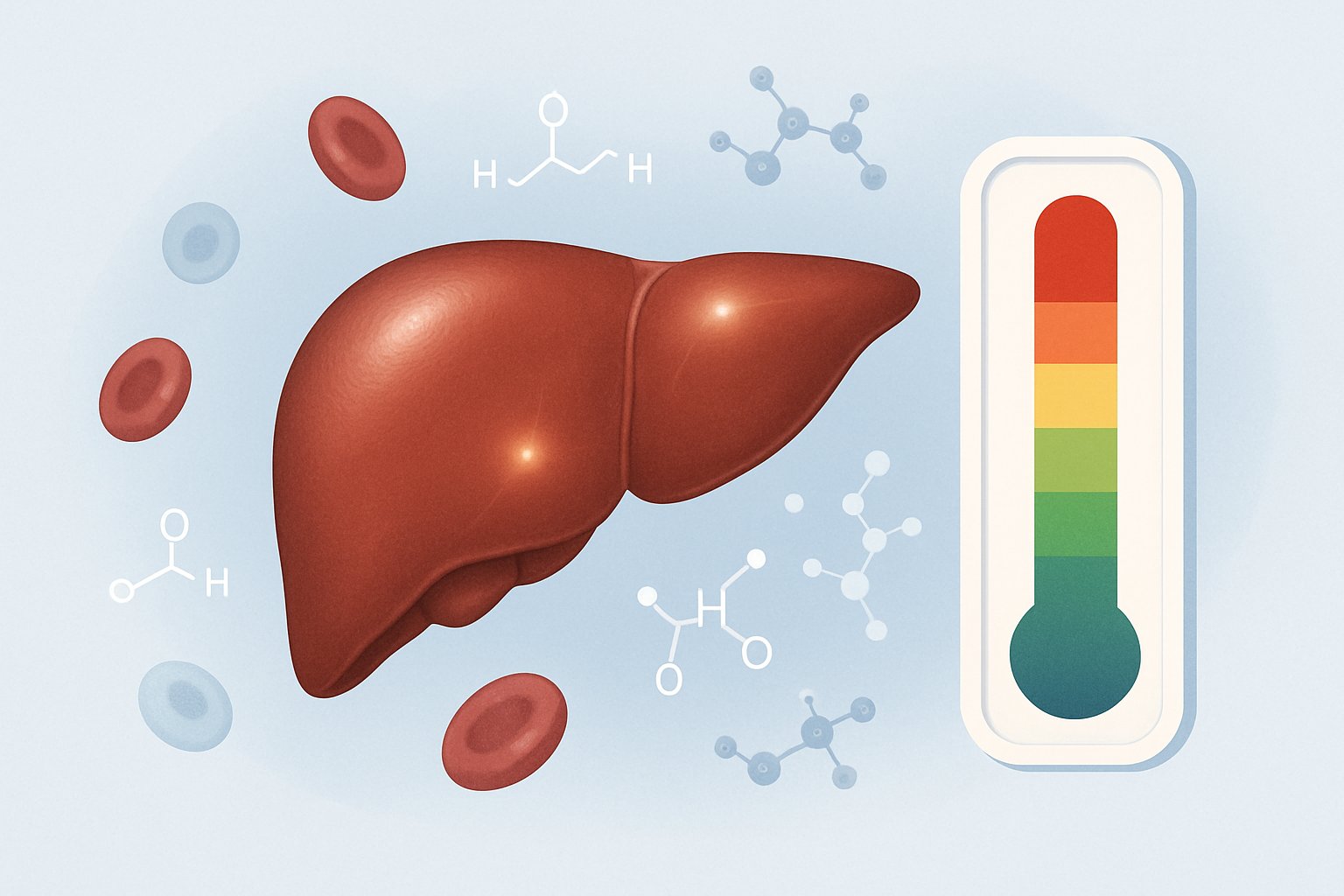
AST is an enzyme that plays a vital role in protein processing and energy production throughout the body. Understanding normal ranges helps identify when elevated levels may signal tissue damage in organs like the liver, heart, or muscles.
Role of Aspartate Aminotransferase in the Body
Aspartate aminotransferase (AST) is an enzyme[3] that helps process proteins by moving parts of amino acids between molecules. This process is essential for creating energy that cells need to function properly.
The enzyme works by transferring a part of aspartate, an amino acid, to another molecule called alpha-ketoglutarate. This creates oxaloacetate and glutamate, which are important building blocks for cellular energy production.
AST is also known as serum glutamic-oxaloacetic transaminase (SGOT) in older medical literature. Both terms refer to the same enzyme that doctors measure in blood tests.
When cells are healthy, they keep most of their AST inside. The enzyme only enters the bloodstream in small amounts during normal cell turnover. This is why healthy people have low AST levels in their blood.
Normal AST Ranges and High AST Levels
Normal AST levels vary by age and gender. Adults typically have AST levels between 0-35 U/L[3], with women often having slightly lower values than men.
Children’s normal ranges:
- 0-5 days: 35-140 U/L
- Under 3 years: 15-60 U/L
- 3-6 years: 15-50 U/L
- 6-12 years: 10-50 U/L
- 12-18 years: 10-40 U/L
Elderly adults may have slightly higher normal values than younger adults. Different laboratories may use slightly different reference ranges for their tests.
When AST levels rise above normal ranges, it usually means that cells containing the enzyme have been damaged or are dying. The higher the AST level, the more extensive the tissue damage may be.
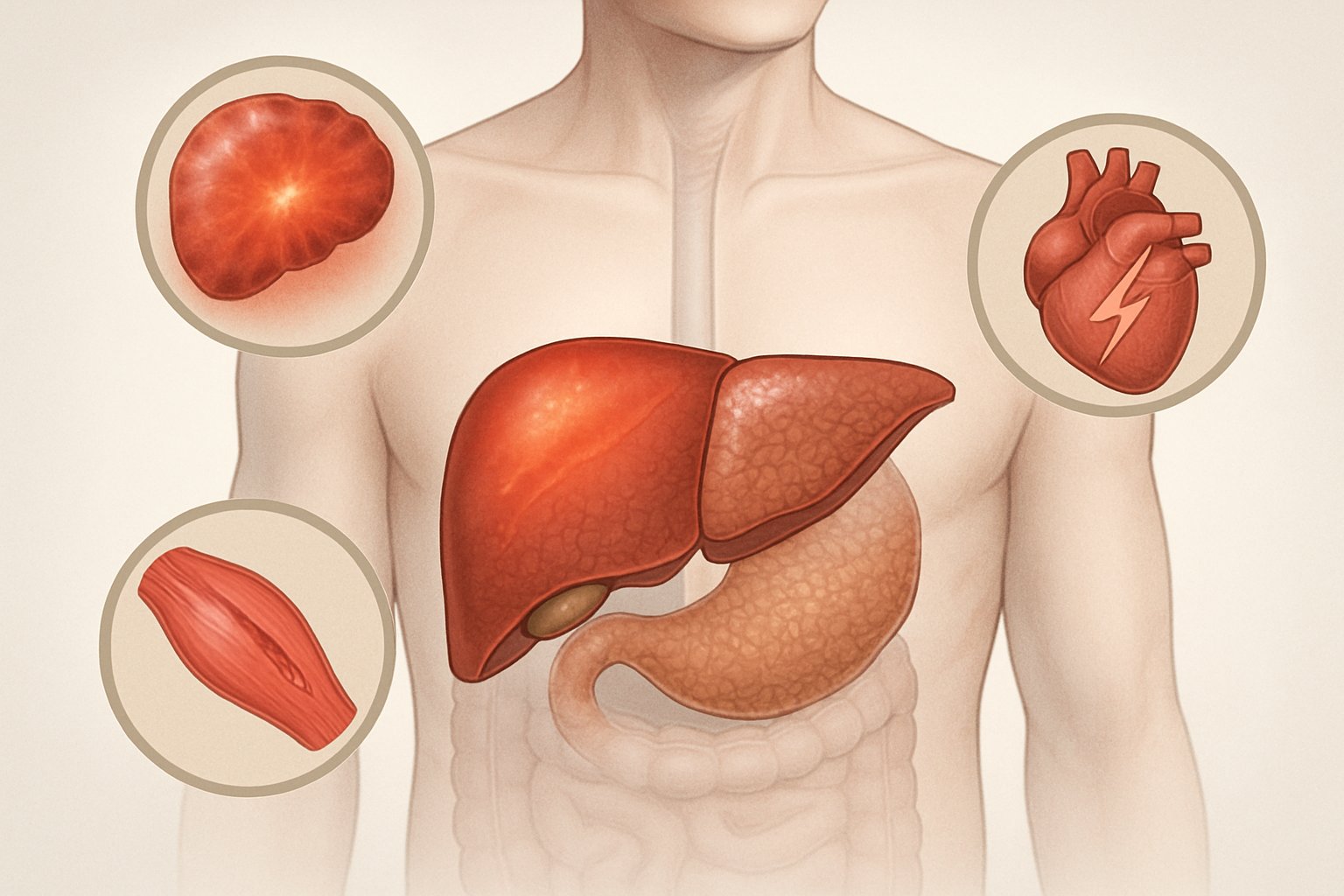
AST as a Liver Enzyme Versus Other Sources
AST is found in your liver, heart, pancreas, muscles and other tissues[4] throughout the body. This makes it different from some other enzymes that come mainly from one organ.
The liver contains high concentrations of AST, which is why doctors often use it to check liver health. However, AST is a non-specific marker because elevated levels can come from damage to any tissue that contains the enzyme.
ALT (alanine aminotransferase) is more specific to the liver than AST. Doctors often compare AST and ALT levels together to better understand where tissue damage is occurring.
When AST levels are much higher than ALT levels, the damage may be coming from the heart, muscles, or other organs rather than just the liver. This ratio helps doctors determine which organs need further testing.
Other liver markers like albumin and bilirubin provide additional information about liver function when evaluated alongside AST results.
Common Causes of High AST Levels
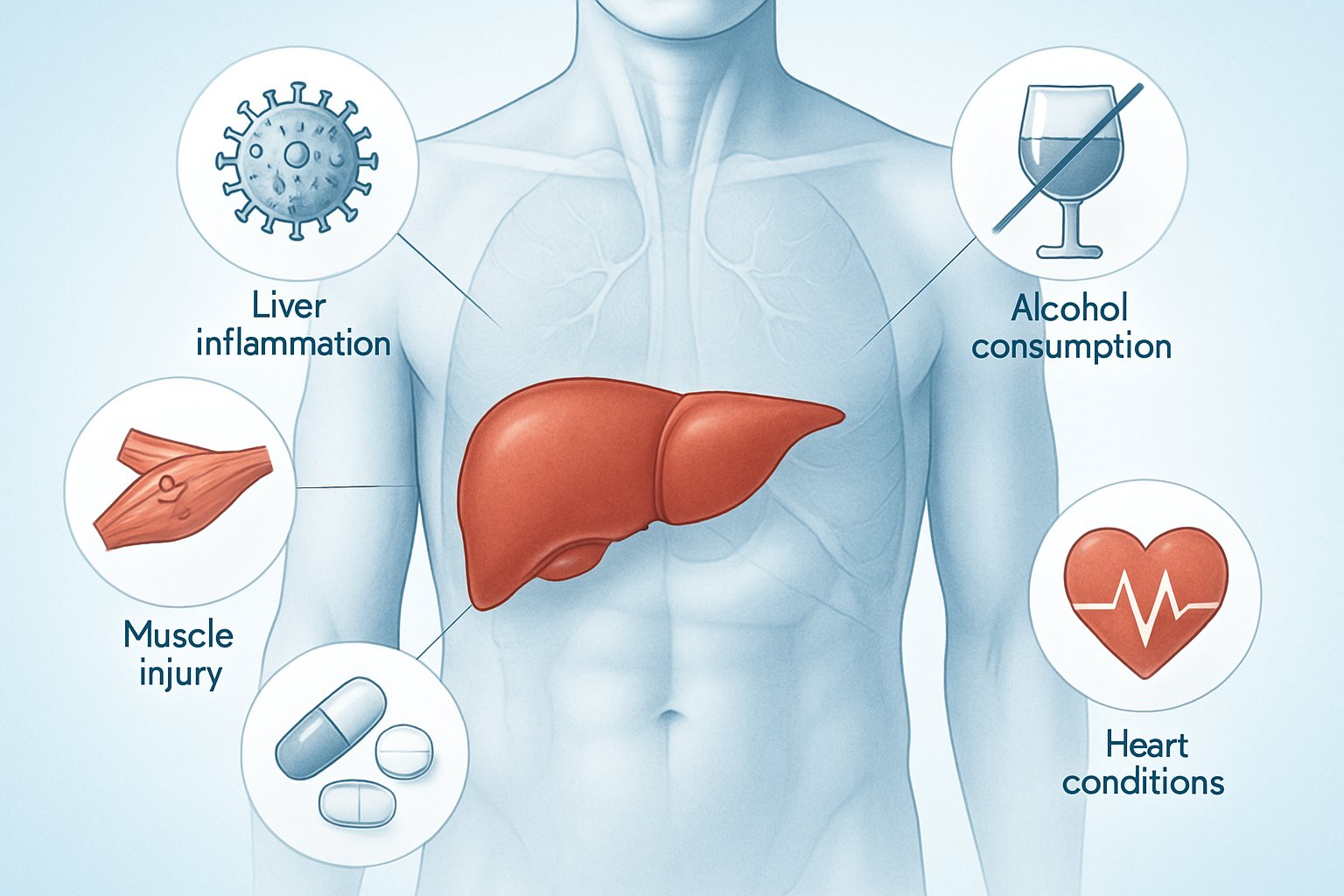
High AST levels can result from liver disease, medication effects, alcohol consumption, and various medical conditions[3] that damage cells throughout the body. The enzyme leaks into the bloodstream when tissues become injured or inflamed.
Liver-Related Conditions and Diseases
Liver conditions represent the most common cause of elevated AST levels[4] since the liver contains high concentrations of this enzyme. Hepatitis from viral infections, autoimmune disorders, or toxic exposure frequently raises AST values.
Nonalcoholic fatty liver disease (NAFLD) and its more severe form, nonalcoholic steatohepatitis (NASH), cause AST elevation as fat accumulates in liver cells. These conditions often develop alongside diabetes and obesity.
Chronic liver diseases that commonly increase AST include:
- Autoimmune hepatitis
- Primary sclerosing cholangitis
- Alpha-1 antitrypsin deficiency
- Hemochromatosis (iron overload)
- Wilson’s disease (copper accumulation)
Liver cancer and cirrhosis represent advanced stages where AST levels may become significantly elevated. Early detection through routine testing helps identify these serious conditions before complications develop.
Alcohol Use and Its Impact on AST
Excessive alcohol consumption damages liver cells and causes AST to leak into the bloodstream[5]. Heavy drinking over time leads to alcoholic fatty liver, which progresses to more serious conditions.
Chronic alcohol use creates inflammation and scarring in liver tissue. This damage releases enzymes like AST into the blood, making it a useful marker for alcohol-related liver problems.
Even moderate alcohol consumption can temporarily raise AST levels in some people. The enzyme typically returns to normal ranges when alcohol use stops, unless permanent liver damage has occurred.
Medications and Toxins Affecting AST
Many prescription and over-the-counter medications can increase AST levels by causing liver cell damage. Statins used for cholesterol management occasionally elevate liver enzymes in sensitive individuals.
Common medications that may raise AST:
- Antibiotics (especially prolonged use)
- Antiviral drugs
- Steroids
- Pain relievers (acetaminophen, NSAIDs)
Herbal supplements like kava and comfrey tea contain compounds toxic to liver cells. These natural products can cause severe liver damage and dramatic AST elevation.
Healthcare providers monitor AST levels when patients take medications known to affect the liver. Regular testing helps detect problems early before serious damage occurs.
Other Medical Conditions Raising AST
AST exists in multiple organs beyond the liver, so various medical conditions can cause elevated levels. Muscle injury from intense exercise, heart attacks, or muscle diseases releases AST into the bloodstream.
Thyroid disorders, particularly hyperthyroidism, can increase AST levels by affecting metabolism and cellular function. Cytomegalovirus infections also commonly raise enzyme levels during active illness.
Non-liver conditions that may elevate AST:
- Heart muscle damage
- Skeletal muscle injury
- Kidney disease
- Pancreatitis
These conditions typically show different patterns of enzyme elevation compared to liver disease. Healthcare providers use additional tests to determine the source of high AST levels.
Interpreting Your AST Results

Understanding AST results requires looking at the actual numbers, comparing them to other liver enzymes like ALT, and considering the degree of elevation. The AST/ALT ratio provides diagnostic clues[6], while the severity of elevation helps determine urgency and potential causes.
AST/ALT Ratio and Its Diagnostic Value
The AST/ALT ratio compares aspartate transaminase levels to alanine transaminase levels. This ratio helps doctors identify specific types of liver damage.
Normal AST/ALT ratio ranges from 0.8 to 1.0 in healthy individuals. When AST levels are higher than ALT levels, the ratio exceeds 1.0.
An AST/ALT ratio above 2.0 often suggests alcoholic liver disease. The ratio above 1.0 but below 2.0 may indicate viral hepatitis or drug-induced liver injury.
Muscle damage can also elevate AST levels without affecting ALT. This creates a high AST/ALT ratio even when the liver is healthy.
Doctors use this ratio alongside other tests like total protein levels and bilirubin. No single liver enzyme test provides a complete picture of liver health.
Significance of Mild, Moderate, and Severe Elevations
AST elevation severity helps determine the urgency of medical attention needed. Different levels suggest different underlying conditions.
Mild elevation (1-3 times normal) ranges from 33-99 U/L. This often occurs with fatty liver disease, medication side effects, or mild hepatitis.
Moderate elevation (3-10 times normal) spans 100-330 U/L. Common causes include viral hepatitis, autoimmune liver disease, or significant alcohol use.
Severe elevation (over 10 times normal) exceeds 330 U/L. This suggests acute liver injury from drug toxicity, viral hepatitis, or heart problems affecting the liver.
Very high AST levels above 1000 U/L require immediate medical attention. These levels often indicate acute liver failure or severe tissue damage.
Limitations of AST and Importance of Context
AST levels alone cannot diagnose specific liver conditions. The enzyme exists in multiple organs including the heart, muscles, and pancreas.
Heart attacks can raise AST levels significantly without any liver involvement. Intense exercise or muscle injuries also elevate AST independently of liver function.
Age, sex, diet, and medications affect AST levels[6]. Recent surgery, burns, or seizures can temporarily increase these liver enzymes.
Doctors need multiple liver function tests for accurate diagnosis. These include ALT, alkaline phosphatase, bilirubin, and total protein measurements.
Normal AST levels don’t guarantee perfect liver health. Some liver diseases progress slowly without dramatically raising enzyme levels initially.
Context matters more than isolated numbers. Symptoms, medical history, and other test results guide proper interpretation of AST levels.
Symptoms and Signs Associated With High AST
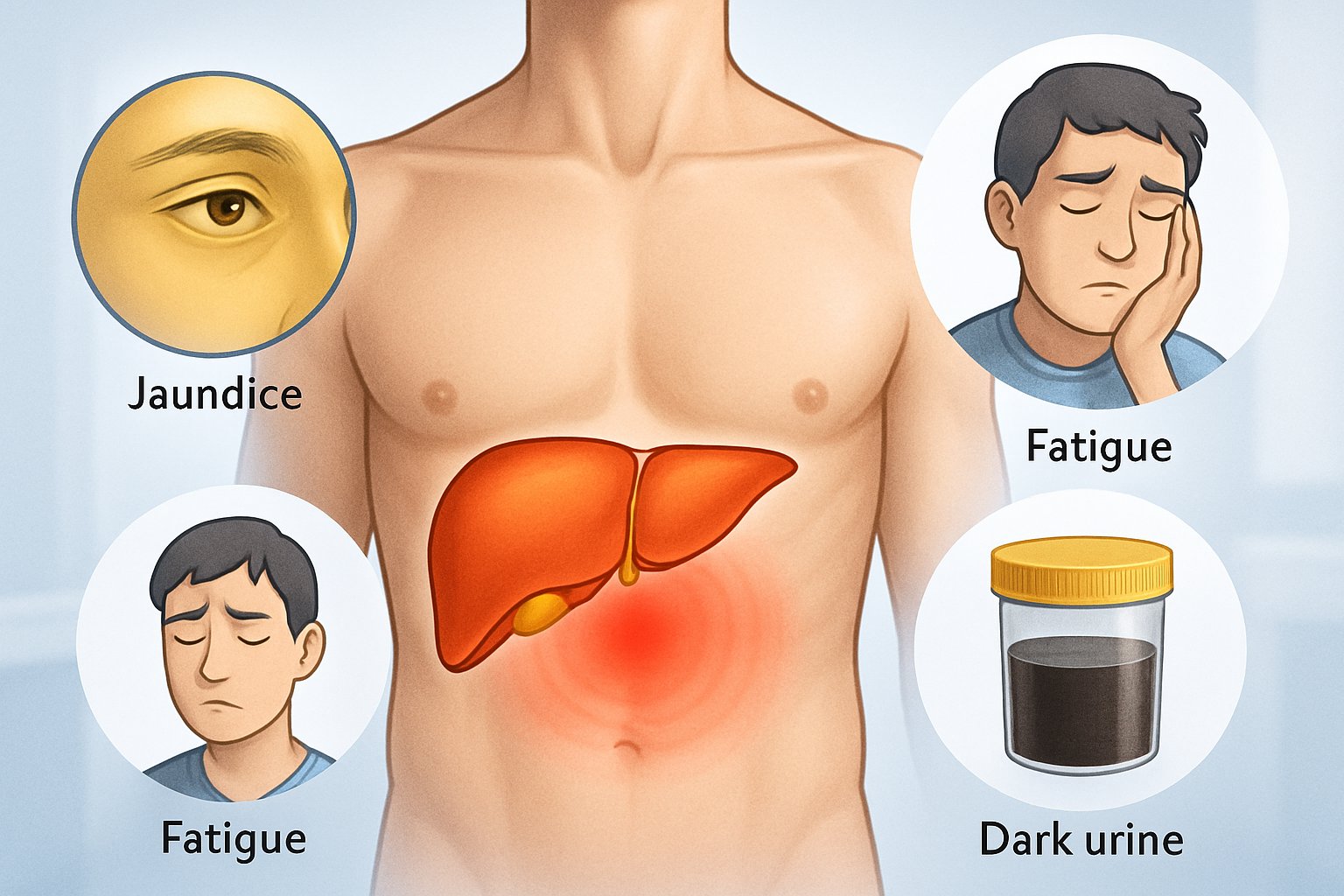
High AST levels often cause no symptoms by themselves, but the underlying conditions that raise AST can produce noticeable physical signs. People may experience digestive issues, skin changes, and energy problems, while those with serious liver disease face more severe complications.
Common Physical Symptoms
Many people with high AST levels notice fatigue and weakness[6] as their first symptoms. This tiredness goes beyond normal exhaustion and does not improve with rest.
Digestive problems appear frequently in patients with elevated AST. Nausea and vomiting[6] can occur along with loss of appetite. Some people lose weight without trying to diet.
Abdominal pain or swelling[6] may develop in the upper right side where the liver sits. This pain can range from mild discomfort to sharp aches.
Common early symptoms include:
- Persistent tiredness that rest does not fix
- Upset stomach and throwing up
- Not wanting to eat food
- Pain in the belly area
- Unexplained weight loss
Signs of Serious Liver or Systemic Conditions
Advanced liver problems cause more obvious warning signs that need immediate medical attention. Jaundice makes the skin and whites of the eyes turn yellow[6]. This happens when bilirubin builds up in the blood.
Dark urine and light-colored stool[6] signal that the liver cannot process waste properly. The urine may look like tea or cola.
Itchy skin affects many people[6] with liver disease. This itching happens all over the body and gets worse at night. Scratching does not provide relief.
Easy bruising or bleeding[6] occurs because the liver cannot make enough clotting proteins. Small cuts may bleed longer than normal.
Serious warning signs:
- Yellow skin or eyes
- Dark brown urine
- Itching that will not stop
- Bruises from minor bumps
- Swollen legs or ankles
Who Is Most at Risk?
People with certain health conditions face higher chances of developing high AST levels. Obesity, diabetes, and high cholesterol[6] increase the risk of fatty liver disease.
Those with alcohol use disorder[6] often develop liver damage that raises AST. Even moderate drinking can cause problems in some people.
Family history of liver disease[6] puts individuals at greater risk. This includes relatives with cirrhosis, liver cancer, or inherited liver conditions.
Certain medications can damage the liver[6]. Acetaminophen causes problems when taken in large amounts. Some supplements and herbs also harm liver cells.
High-risk groups:
- People with excess body weight
- Those who drink alcohol regularly
- Patients taking liver-toxic medications
- Individuals with family liver disease history
- People exposed to hepatitis viruses
How High AST Is Diagnosed and Assessed
Doctors use several tests to diagnose high AST levels and determine the cause. Blood tests check liver function, while imaging studies look at liver structure and condition.
Key Blood Tests and Liver Function Tests
The AST test measures enzyme levels[4] in the blood to check for liver damage. Normal AST levels range from 8 to 33 units per liter.
Doctors often order a complete liver panel alongside the AST test. This includes the ALT test, which measures another liver enzyme called alanine aminotransferase.
Key liver function tests include:
- AST (aspartate aminotransferase)
- ALT (alanine aminotransferase)
- ALP (alkaline phosphatase)
- Bilirubin levels
- Albumin protein levels
The ALT test helps doctors tell if liver damage is the main cause of high AST. High AST with normal ALT might point to heart or muscle problems instead of liver issues.
Doctors also check the AST to ALT ratio. A ratio above 2:1 often suggests alcohol-related liver damage.
Imaging Studies for Liver Evaluation
Imaging tests help doctors see the liver’s size, shape, and condition. These tests show structural problems that blood tests might miss.
Ultrasound is usually the first imaging test ordered. It uses sound waves to create pictures of the liver. Ultrasound can detect fatty liver disease, tumors, and fluid buildup.
CT scans provide more detailed images than ultrasound. They can spot liver scarring, tumors, and blood vessel problems. CT scans use X-rays and contrast dye for clearer pictures.
MRI scans give the most detailed liver images. They help doctors see liver tissue damage and blood flow problems. MRI is best for finding small tumors or checking liver function.
These imaging tests are painless and help doctors plan treatment. They also track how well treatments are working over time.
Role of Liver Biopsy
A liver biopsy removes a small piece of liver tissue for testing. Doctors use this test when other methods don’t give clear answers about liver damage.
The biopsy shows the exact type and amount of liver damage. It can detect inflammation, scarring, and fat buildup in liver cells.
Two main types of liver biopsy:
- Needle biopsy through the skin
- Laparoscopic biopsy during surgery
Doctors usually try other tests first before doing a biopsy. The procedure has small risks like bleeding or infection.
A biopsy helps doctors stage liver disease and pick the best treatment. It’s most helpful for checking hepatitis, cirrhosis, and unknown liver problems.
Comprehensive Metabolic Panel and Other Assessments
The comprehensive metabolic panel includes AST testing[4] along with other important blood markers. This panel checks kidney function, blood sugar, and electrolyte levels.
The panel typically includes:
- Glucose levels
- Kidney function markers
- Protein levels
- Electrolyte balance
- Liver enzymes including AST
Doctors also check for hepatitis viruses, which are common causes of high AST. Blood tests can detect hepatitis A, B, and C infections.
Additional tests might include iron levels, autoimmune markers, and drug screening. These help find specific causes of liver damage.
Regular screening helps catch liver problems early. People with risk factors like diabetes or alcohol use need more frequent testing.
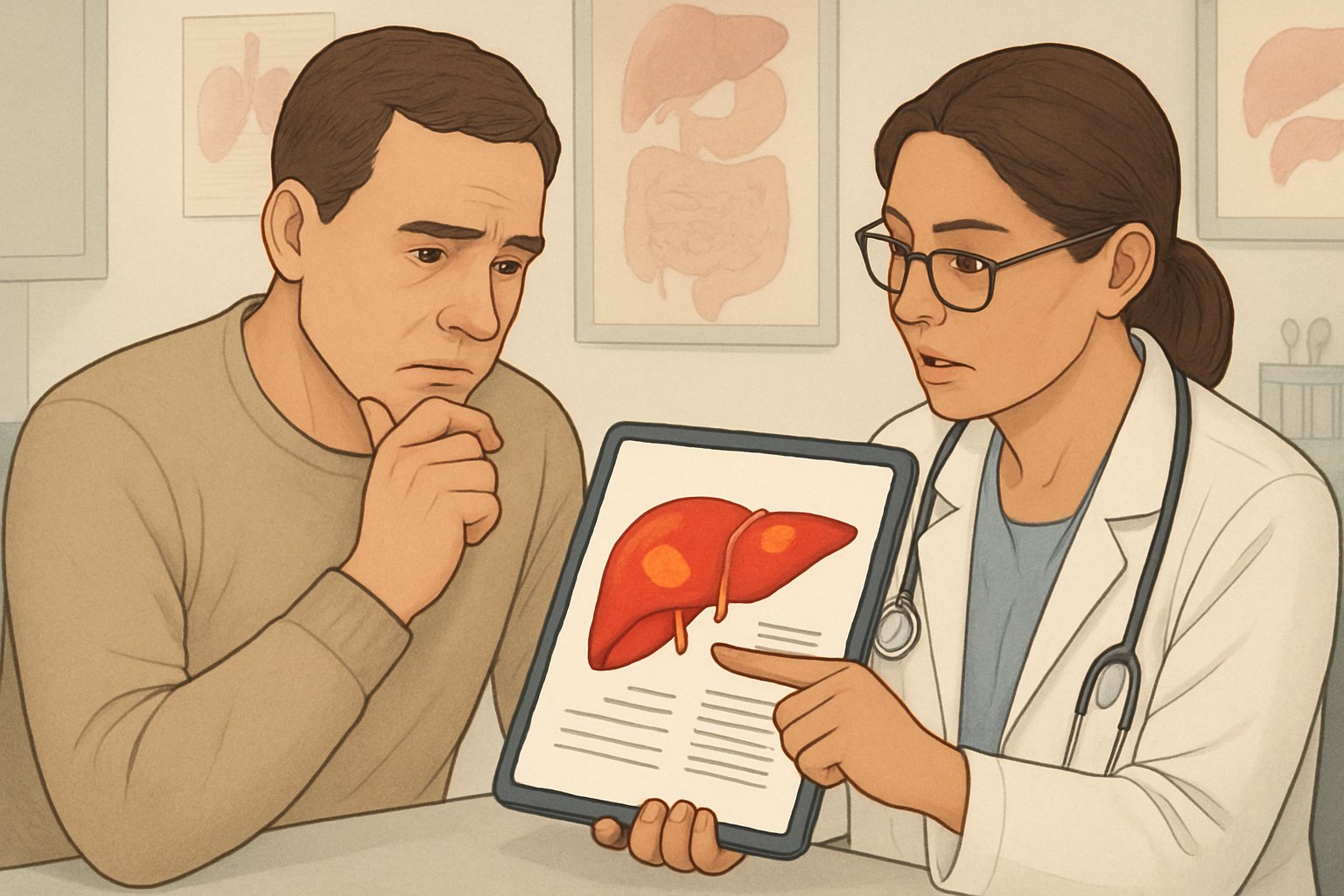
Management and Next Steps If Your AST Is High
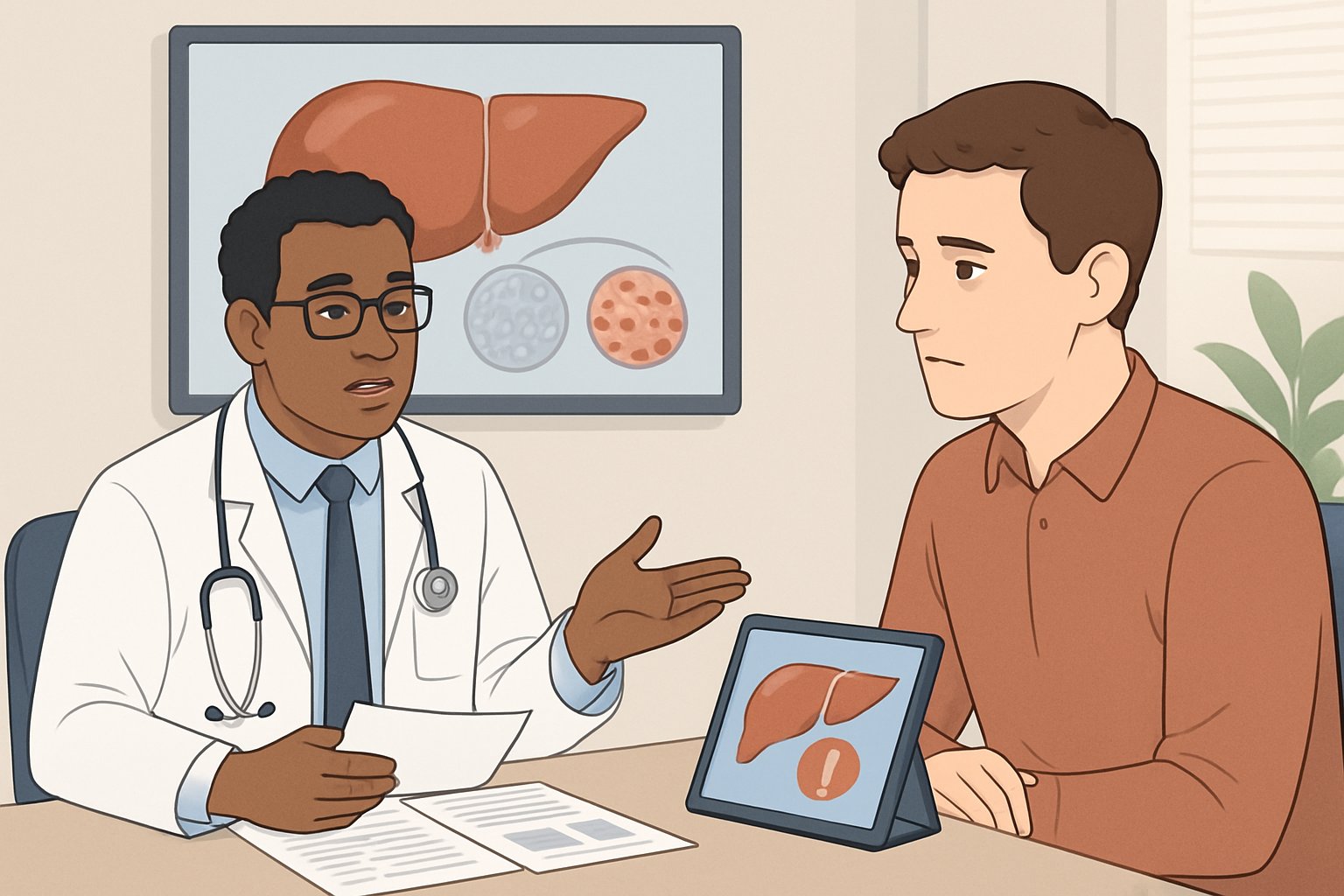
When AST levels are elevated, doctors focus on finding and treating the root cause while supporting overall liver health. Treatment plans typically include addressing specific conditions, making lifestyle changes, and regular monitoring to track progress.
Addressing Underlying Causes
The first step involves identifying what caused the elevated AST levels. Doctors may need to assess underlying liver disease, medications, and other risk factors[7] through detailed history and physical examination.
Common causes requiring specific treatment:
- Alcoholic liver disease: Complete alcohol cessation
- MASLD (Metabolic dysfunction-associated steatotic liver disease): Managing diabetes and metabolic conditions
- Fatty liver disease: Weight reduction and dietary changes
- Medication-induced liver injury: Stopping or changing problematic medications
- Viral hepatitis: Antiviral treatments when appropriate
Healthcare providers may order additional blood tests, imaging studies, or liver biopsies. These tests help determine the exact cause and severity of liver damage.
Some patients need immediate treatment for serious conditions. Others may find their levels return to normal once the underlying problem is addressed.
Lifestyle Modifications to Support Liver Health
Several lifestyle changes can help improve liver health and lower AST levels naturally. These modifications work best when combined with medical treatment for underlying conditions.
Weight management plays a crucial role, especially for patients with fatty liver disease or MASLD. Losing 7-10% of body weight can significantly reduce liver fat and inflammation.
Physical activity should include both cardio and strength training exercises. Regular exercise helps with weight loss and reduces liver fat even without significant weight changes.
Dietary changes that support liver function include:
- Limiting processed foods and added sugars
- Reducing saturated fats
- Increasing fruits, vegetables, and whole grains
- Limiting sodium intake
Avoiding harmful substances is essential. This means stopping smoking completely and eliminating alcohol consumption, especially for those with alcoholic liver disease.
Patients should also review all medications and supplements with their doctor. Some over-the-counter drugs and herbal supplements can damage the liver.
Monitoring and Follow-Up Care
Regular monitoring helps track whether treatments are working and AST levels are improving. Most elevated liver enzymes are temporary and resolve on their own[8], but some cases need ongoing medical attention.
Follow-up blood tests are typically done every 3-6 months initially. The frequency depends on how high the AST levels were and what caused them.
Monitoring schedule may include:
- Blood tests to check AST, ALT, and other liver enzymes
- Tests for liver function and overall health
- Imaging studies like ultrasounds when needed
Patients should watch for symptoms that might indicate worsening liver problems. These include yellowing of skin or eyes, severe fatigue, abdominal pain, or unusual bleeding.
Healthcare providers may refer patients to liver specialists if AST levels remain high despite treatment. Some people need long-term management to prevent further liver damage.
Regular check-ups help catch problems early and adjust treatment plans as needed. Patients who follow their treatment plans often see significant improvement in their liver enzyme levels.
Potential Complications of Persistently High AST
When AST levels remain elevated over time, serious complications can develop. The most concerning risks include progressive liver disease that may lead to complete organ failure and other systemic health problems that affect multiple body systems.
Progression of Liver Disease and Liver Failure
Chronic elevation of AST often signals ongoing liver inflammation that can worsen without proper treatment. This persistent liver damage may progress through several stages.
Early Stage Complications:
- Chronic hepatitis develops when inflammation continues for months or years
- Liver cells die and get replaced by scar tissue
- Normal liver function begins to decline gradually
Advanced Disease Progression: The liver may progress to cirrhosis, where healthy tissue becomes replaced by permanent scar tissue. This scarring blocks blood flow through the liver and prevents it from working properly.
Critical Stage Risks:
- Complete liver failure can occur when the organ can no longer perform essential functions
- Toxins build up in the blood when the liver cannot filter them
- Blood clotting problems develop because the liver produces fewer clotting proteins
People with high AST levels above 200 U/L may indicate severe liver damage[1]. Early intervention helps prevent progression to these serious stages.
Other Long-Term Health Risks
Persistently high liver enzymes create risks beyond liver-specific problems. These complications affect other organs and body systems.
Cardiovascular Complications:
- Heart problems may develop because the liver helps process cholesterol and fats
- Blood pressure can become harder to control
- Risk of heart attack increases with severe liver dysfunction
Metabolic Disruptions: The liver plays a key role in processing nutrients and medications. When it does not work well, blood sugar control becomes difficult. Protein levels in blood may drop dangerously low.
Immune System Problems: A damaged liver cannot fight infections as effectively. People become more likely to get sick from bacteria and viruses. Wounds may heal more slowly than normal.
Digestive Issues:
- Bile production decreases, making it hard to digest fats
- Fluid can build up in the abdomen
- Bleeding in the digestive tract may occur due to increased pressure in liver blood vessels
Frequently Asked Questions
High AST levels can result from liver damage, muscle injury, or other medical conditions. Understanding the specific causes, health implications, and treatment approaches helps patients make informed decisions about their care.
What factors can lead to elevated AST levels?
Several health conditions can cause high AST levels[6] beyond liver disease. Heart problems, muscle disorders, and thyroid disease commonly raise AST readings.
Certain medications increase AST levels, particularly those that can damage the liver. Acetaminophen is a common example of a drug that affects liver enzymes when taken in large amounts.
Physical activities and medical procedures also impact AST readings. Recent surgery, intense exercise, or sustaining burns can temporarily elevate these enzyme levels.
Medical events like seizures or heat stroke cause AST to rise. Pregnancy and some infections, including mononucleosis, also lead to higher readings.
How does an increase in AST indicate liver function issues?
AST is primarily found in liver cells, so damage to these cells releases the enzyme into the bloodstream. When liver tissue becomes injured or inflamed, AST levels rise above the normal range of 8 to 33 units per liter.
Higher AST readings suggest that liver cells are being destroyed faster than normal. This process occurs in conditions like hepatitis, cirrhosis, and fatty liver disease.
The degree of AST elevation often corresponds to the extent of liver damage. However, AST levels alone cannot determine the specific type of liver disease present.
What conditions are associated with concurrently high levels of AST and ALT?
Liver diseases typically cause both AST and ALT levels to rise together. Hepatitis, whether viral or caused by alcohol, commonly elevates both enzymes simultaneously.
Fatty liver disease raises both AST and ALT readings. This condition often develops in people with obesity, diabetes, or high cholesterol levels.
Drug-induced liver injury frequently increases both enzymes. Certain medications, herbal supplements, and toxins can damage liver cells and raise both AST and ALT.
Cirrhosis and other chronic liver conditions usually show elevated levels of both enzymes. The pattern of elevation can help doctors determine the specific liver condition.
How do varying AST levels affect health risks?
Mildly elevated AST levels may indicate early liver damage or muscle injury. These readings often require monitoring but may not need immediate treatment.
Significantly high AST levels suggest more serious liver damage or disease. These readings typically require further testing and medical evaluation to determine the underlying cause.
Very high AST levels can indicate acute liver failure or severe liver damage. This situation requires immediate medical attention and treatment.
Low AST levels are generally less concerning but may indicate health issues in some cases. Studies show that very low AST levels in older men may be associated with increased mortality risk.
At what point should elevated liver enzymes be a cause for concern?
AST levels above 33 units per liter warrant medical attention and further evaluation. However, the degree of concern depends on how high the levels are and other symptoms present.
Persistent elevation over several weeks or months indicates a need for additional testing. Single elevated readings may be temporary and not necessarily concerning.
Symptoms like jaundice, abdominal pain, or unexplained fatigue[6] combined with high AST levels require immediate medical evaluation. These signs may indicate serious liver problems.
People with risk factors for liver disease should take any AST elevation seriously. Risk factors include alcohol use, family history of liver disease, or exposure to hepatitis.
How are abnormal AST levels managed and treated?
Treatment for high AST levels focuses on addressing the underlying cause rather than the enzyme levels themselves. Liver diseases require specific treatments based on the type and severity of the condition.
Lifestyle changes can help lower AST levels when liver disease is present. Reducing alcohol consumption, maintaining a healthy weight, and eating a diet rich in fruits and vegetables support liver health.
Medication adjustments may be necessary if drugs are causing elevated AST levels. Doctors may switch to alternative medications that do not affect liver function.
Regular monitoring helps track progress and treatment effectiveness. Follow-up blood tests determine whether AST levels are improving with treatment and lifestyle changes.
References
- What Level Of AST Is Dangerous - Understanding the Risks and Implications. https://statcarewalkin.com/info/what-level-of-ast-is-dangerous.html Accessed October 27, 2025
- Elevated Liver Enzymes: What Is It, Causes, Prevention & Treatment. https://my.clevelandclinic.org/health/symptoms/17679-elevated-liver-enzymes Accessed October 27, 2025
- Understanding High AST Levels: Causes and Implications. https://www.rupahealth.com/post/understanding-high-ast-levels-causes-and-implications Accessed October 27, 2025
- Aspartate Transferase (AST) Blood Test: What It Is, Procedure & Results. https://my.clevelandclinic.org/health/diagnostics/22147-aspartate-transferase-ast Accessed October 27, 2025
- High AST Levels: Causes, Treatment, and Prevention. https://www.personalabs.com/blog/high-ast-levels-causes-treatment-and-prevention/ Accessed October 27, 2025
- AST/ALT ratio provides diagnostic clues. https://www.verywellhealth.com/ast-sgot-8411027 Accessed October 27, 2025
- How to approach elevated liver enzymes?. https://www.aasld.org/liver-fellow-network/core-series/back-basics/how-approach-elevated-liver-enzymes Accessed October 27, 2025
- Most elevated liver enzymes are temporary and resolve on their own. https://www.verywellhealth.com/elevated-liver-enzymes-5443042 Accessed October 27, 2025
