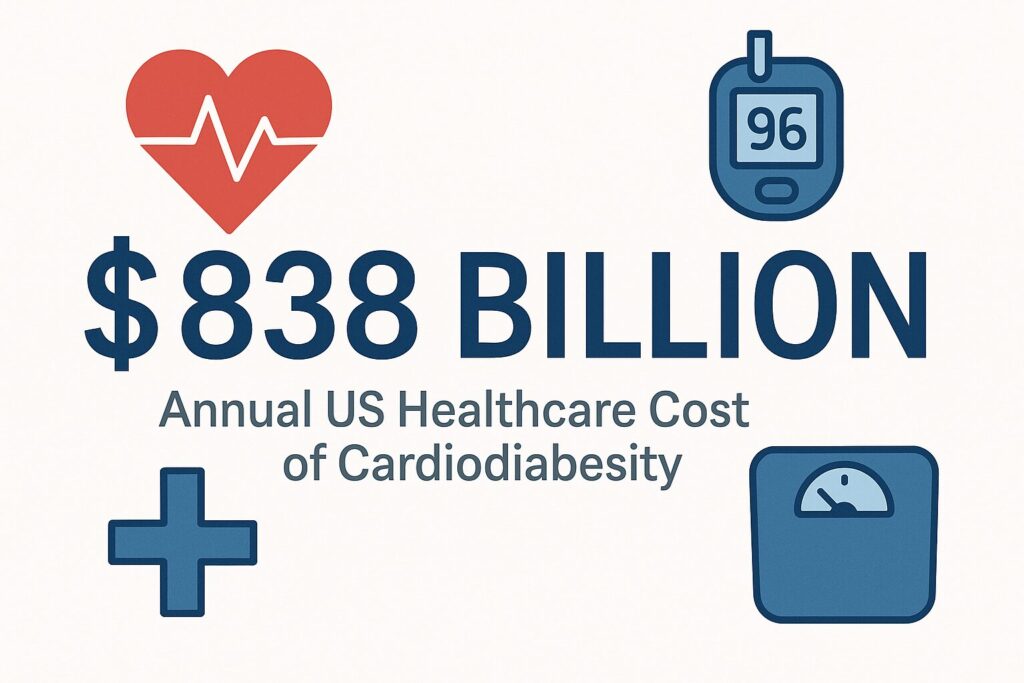
Cardiodiabesity represents a hybrid medical term that describes the intricate and synergistic relationship between cardiovascular disease (CVD), type 2 diabetes mellitus (T2DM), and obesity—three of the most significant health challenges of our time. This concept emerged from the recognition that these conditions frequently coexist, share common pathophysiological mechanisms, and create a compounding effect that dramatically increases morbidity, mortality, and healthcare costs. The term builds upon earlier concepts like “diabesity” (coined by former US Surgeon General C. Everett Koop) and evolved to encompass the cardiovascular dimension, acknowledging that diabetes should be viewed as a vascular disease from its onset. With an estimated economic burden of $838 billion annually in the United States alone, cardiodiabesity has become one of the most pressing public health crises, affecting millions of individuals worldwide and representing a progressive disease that significantly impacts both individual health outcomes and healthcare system resources.
Conceptual Framework and Evolution
Cardiodiabesity encompasses the complex interrelationship between cardiovascular disease, type 2 diabetes, and obesity, recognizing that these conditions are not merely coincidental comorbidities but represent interconnected pathophysiological processes. The term was first introduced in medical literature around 2008 in the British Journal of Cardiology, when cardiologists began emphasizing that diabetes should be viewed as a vascular disease from the outset. This paradigm shift acknowledged the clustering of vascular risk factors associated with insulin resistance, including visceral obesity, dyslipidemia, and hypertension, which collectively contribute to accelerated cardiovascular disease development.[1]
The European Society of Cardiology-European Association for the Study of Diabetes (ESC-EASD) guidelines have established the close relationship between hyperglycemia and microvascular disease, emphasizing that cardiovascular risk appears early, prior to the development of T2DM. This recognition has led to the recommendation that patients with T2DM should be managed as patients with established atherosclerotic disease from diagnosis, fundamentally changing treatment approaches and risk stratification strategies.[2]
Clinical Relevance and Disease Burden
The clinical significance of cardiodiabesity extends beyond the simple additive effects of its individual components. Research demonstrates that less than 7% of the U.S. adult population has optimal cardiometabolic health, indicating the widespread prevalence of risk factors that predispose to cardiodiabesity. The condition represents a progressive disease process with distinct stages, each associated with increasing healthcare utilization and costs.[3]
Current epidemiological data reveals that cardiovascular disease affects 127.9 million U.S. adults (48.6%), while 29.3 million adults (10.6%) have diagnosed diabetes and 41.9% of adults are obese. The intersection of these conditions creates a population at extremely high risk for adverse outcomes, with studies showing that individuals with all three conditions have dramatically increased rates of complications and mortality compared to those with individual conditions.[4]
Cardiodiabesity: Understanding the Triple Threat of Modern Chronic Disease
Cardiodiabesity represents a hybrid medical term that describes the intricate and synergistic relationship between cardiovascular disease (CVD), type 2 diabetes mellitus (T2DM), and obesity—three of the most significant health challenges of our time. This concept emerged from the recognition that these conditions frequently coexist, share common pathophysiological mechanisms, and create a compounding effect that dramatically increases morbidity, mortality, and healthcare costs. The term builds upon earlier concepts like “diabesity” (coined by former US Surgeon General C. Everett Koop) and evolved to encompass the cardiovascular dimension, acknowledging that diabetes should be viewed as a vascular disease from its onset. With an estimated economic burden of $838 billion annually in the United States alone, cardiodiabesity has become one of the most pressing public health crises, affecting millions of individuals worldwide and representing a progressive disease that significantly impacts both individual health outcomes and healthcare system resources.[1]
Defining Cardiodiabesity and Its Clinical Significance
Conceptual Framework and Evolution
Cardiodiabesity encompasses the complex interrelationship between cardiovascular disease, type 2 diabetes, and obesity, recognizing that these conditions are not merely coincidental comorbidities but represent interconnected pathophysiological processes. The term was first introduced in medical literature around 2008 in the British Journal of Cardiology, when cardiologists began emphasizing that diabetes should be viewed as a vascular disease from the outset. This paradigm shift acknowledged the clustering of vascular risk factors associated with insulin resistance, including visceral obesity, dyslipidemia, and hypertension, which collectively contribute to accelerated cardiovascular disease development.[1]
The European Society of Cardiology-European Association for the Study of Diabetes (ESC-EASD) guidelines have established the close relationship between hyperglycemia and microvascular disease, emphasizing that cardiovascular risk appears early, prior to the development of T2DM. This recognition has led to the recommendation that patients with T2DM should be managed as patients with established atherosclerotic disease from diagnosis, fundamentally changing treatment approaches and risk stratification strategies.[2]
Clinical Relevance and Disease Burden
The clinical significance of cardiodiabesity extends beyond the simple additive effects of its individual components. Research demonstrates that less than 7% of the U.S. adult population has optimal cardiometabolic health, indicating the widespread prevalence of risk factors that predispose to cardiodiabesity. The condition represents a progressive disease process with distinct stages, each associated with increasing healthcare utilization and costs.
Current epidemiological data reveals that cardiovascular disease affects 127.9 million U.S. adults (48.6%), while 29.3 million adults (10.6%) have diagnosed diabetes and 41.9% of adults are obese. The intersection of these conditions creates a population at extremely high risk for adverse outcomes, with studies showing that individuals with all three conditions have dramatically increased rates of complications and mortality compared to those with individual conditions.[4]
Pathophysiological Mechanisms and Disease Progression
Molecular and Cellular Pathways
The pathophysiology of cardiodiabesity involves multiple interconnected molecular mechanisms that create a self-perpetuating cycle of metabolic dysfunction. Central to this process is insulin resistance, which serves as a common denominator linking obesity, diabetes, and cardiovascular disease. Visceral white adipose tissue (WAT) dysfunction plays a pivotal role, leading to increased production of pro-inflammatory adipokines, oxidative stress, and activation of the renin-angiotensin-aldosterone system (RAAS).[5]
Chronic inflammation represents a key pathophysiological mechanism in cardiodiabesity. Adipose tissue inflammation leads to reduced production of protective adiponectin while increasing secretion of harmful adipokines such as resistin and leptin, along with pro-inflammatory cytokines. This inflammatory milieu contributes to endothelial dysfunction, vascular stiffness, and impaired vascular relaxation, ultimately leading to cardiac diastolic dysfunction and increased cardiovascular risk.[6]
The activation of the RAAS system in obesity represents another critical pathway. Under pathophysiological conditions, RAAS stimulates inflammation and structural remodeling, inducing cardiac and vascular injury through the actions of angiotensin II, transforming growth factor beta (TGF-β), and insulin-like growth factors (IGFs). This leads to excessive collagen deposition in cardiac tissue, contributing to left ventricular hypertrophy, fibrosis, and eventual heart failure.[6]
Metabolic Substrate Utilization and Cardiac Effects
Cardiodiabesity significantly alters myocardial substrate metabolism, with obesity and T2DM inducing changes in substrate utilization that negatively impact cardiac function. The condition is characterized by increased free fatty acid (FFA) uptake and β-oxidation in the heart, which has deleterious effects on cardiac contractile function. These metabolic changes, combined with oxidative stress and inflammation, promote left ventricular hypertrophy, fibrosis, arrhythmias, and heart failure—particularly heart failure with preserved ejection fraction (HFpEF).[6]
Epicardial adipose tissue (EAT) accumulation represents a unique feature of cardiodiabesity. EAT is strongly correlated with visceral obesity and exerts local negative effects on the myocardium through natural compression, local delivery of free fatty acids and cardioactive hormones, and release of pro-inflammatory adipokines. Increased EAT volume is independently associated with increased myocardial fat content, interstitial myocardial fibrosis, coronary calcification, and atheromatous plaque formation.[6]
Microvascular Dysfunction and Atherosclerosis
Cardiodiabesity is associated with significant microvascular dysfunction across multiple organ systems. In the coronary circulation, this manifests as reduced coronary vasodilator responsiveness and diminished coronary flow reserve, which serves as a powerful predictor of major adverse cardiovascular events. These microvascular changes occur prior to overt atherosclerotic disease and contribute to reductions in cardiac contractile function and concentric ventricular hypertrophy.[5]
The atherosclerotic process in cardiodiabesity is accelerated and more aggressive than in non-cardiometabolic populations. Studies show approximately a 2-fold increase in risk of myocardial infarction and significantly elevated cardiovascular mortality. The PROSPECT study revealed compositional differences in coronary plaques from patients with metabolic syndrome, showing increased prevalence of adverse features including total plaque burden, necrotic core, and calcium content.[5]
Epidemiology and Disease Stages
Population Prevalence and Demographics
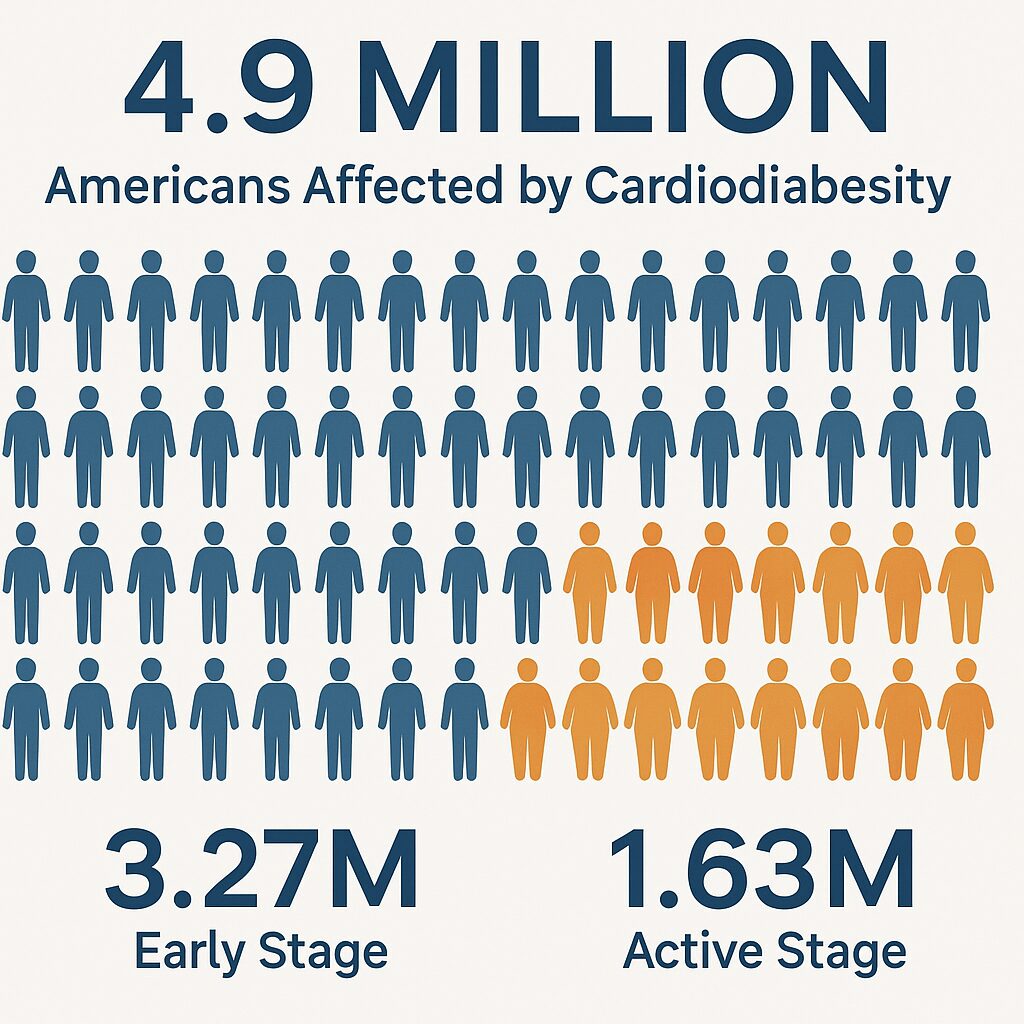
Recent comprehensive analyses reveal the substantial epidemiological burden of cardiodiabesity in the United States. A large-scale study examining over 4.9 million patients identified 3,273,813 patients with at least one early-stage cardiodiabesity condition and 1,628,407 patients with active cardiodiabesity. These numbers represent a significant portion of the adult population and highlight the widespread nature of this health crisis.
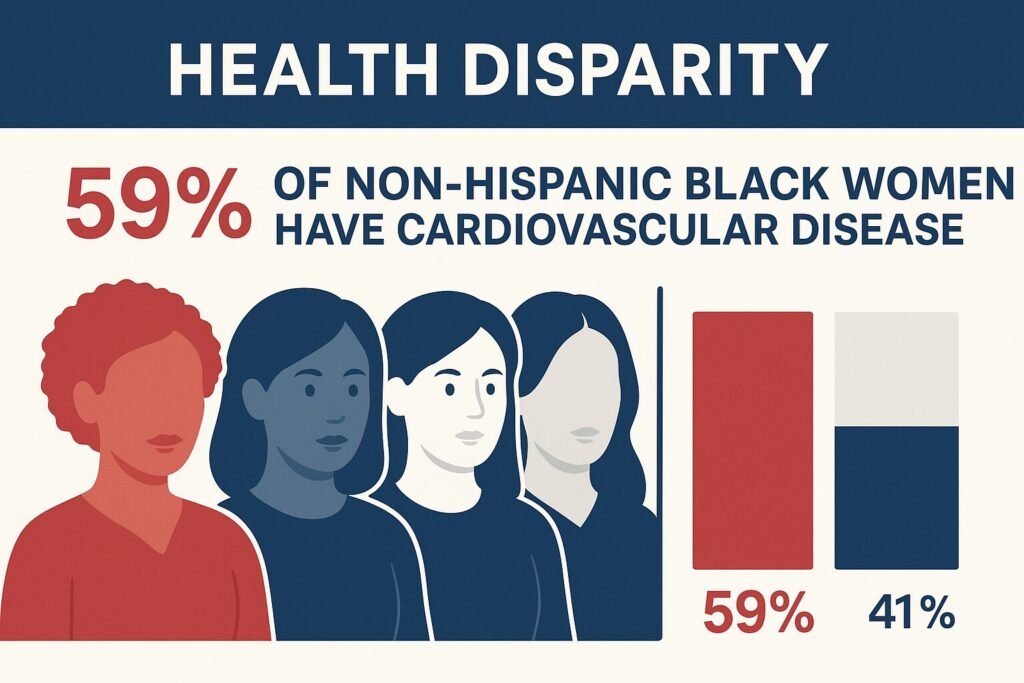
Demographic disparities are evident in cardiodiabesity prevalence, with certain populations bearing disproportionate burdens. Between 2017 and 2020, 59.0% of non-Hispanic Black females and 58.9% of non-Hispanic Black males had some form of CVD, representing the highest prevalence among all racial and ethnic groups. These disparities extend to the individual components of cardiodiabesity, with higher rates of diabetes, obesity, and hypertension observed in minority populations.[7]
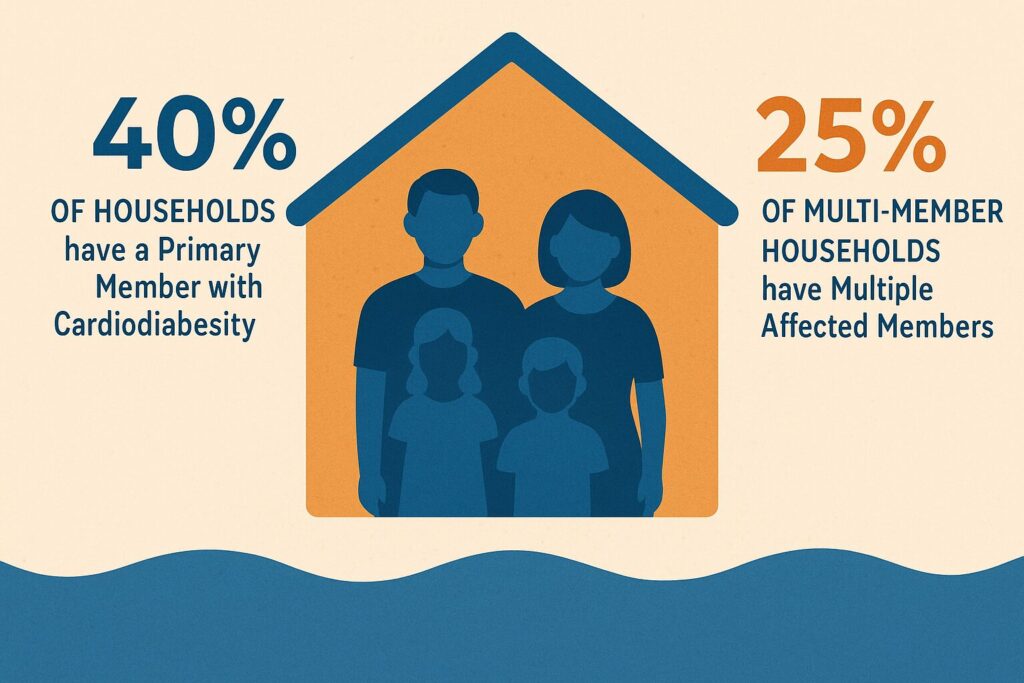
Household-level analysis reveals that cardiodiabesity has familial clustering patterns, with 40% of households having a primary member with cardiodiabesity and 25% of multi-member households having more than one person with the condition. This finding suggests both genetic and environmental factors contribute to cardiodiabesity development and supports the need for family-centered intervention approaches.
Three-Stage Disease Progression Model
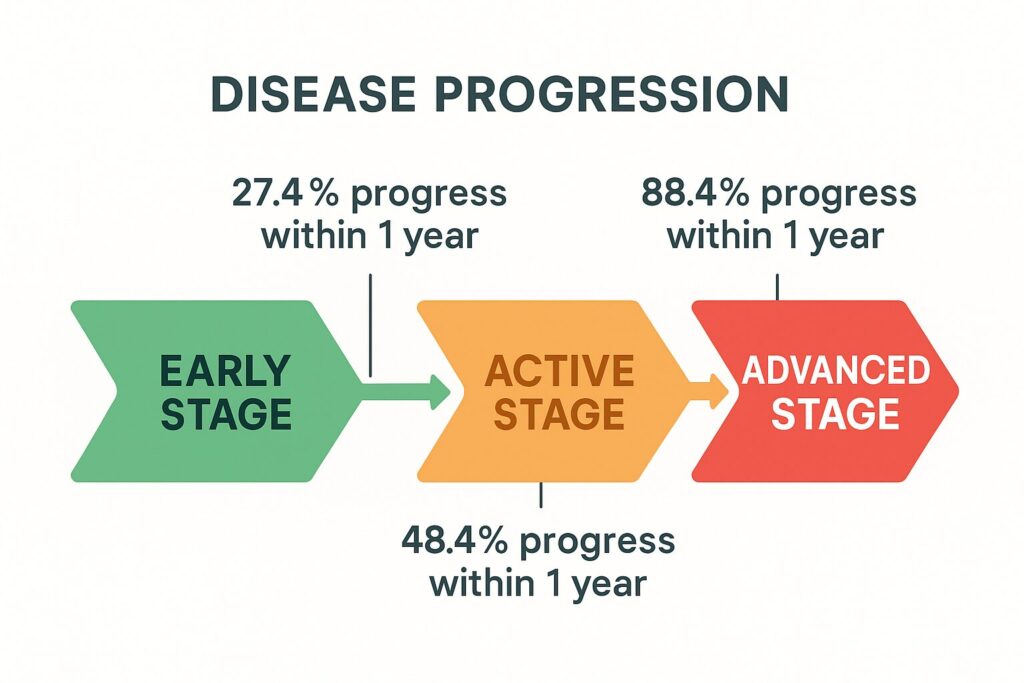
Recent research has established cardiodiabesity as a progressive disease with three distinct stages: early-stage (at-risk), active (diagnosed), and advanced (complicated). This staging system provides a framework for understanding disease progression and developing targeted interventions.[3]
Early-Stage Cardiodiabesity is characterized by risk factors and precursor conditions including hypertension, hyperlipidemia, prediabetes, overweight status (BMI 25-29.9), and chronic kidney disease stages 1-2. Among individuals with all early-stage conditions, 27.4% progress to active cardiodiabesity within one year. Key predictors of progression include hypertension (OR: 2.31), hyperlipidemia (OR: 1.77), CKD stages 1-2 (OR: 1.74), prediabetes (OR: 1.64), and living in areas with high social needs (OR: 1.25).[9]
Active Cardiodiabesity involves diagnosed cardiovascular disease, type 2 diabetes, and/or obesity. This stage represents established disease requiring active medical management. Remarkably, 88.4% of patients with all active cardiodiabesity conditions progress to complications within one year, highlighting the rapid and aggressive nature of disease progression. Predictors of progression to advanced stages include T2D (OR: 1.88), CVD (OR: 1.47), CKD stages 3-4 (OR: 1.37), and obesity (OR: 1.29).[3]
Advanced Cardiodiabesity encompasses severe complications and end-organ damage, including heart failure, myocardial infarction, stroke, kidney failure, and other cardiovascular complications. This stage is associated with the highest healthcare utilization, costs, and mortality rates.
Clinical Manifestations and Complications
Cardiovascular Complications
The cardiovascular manifestations of cardiodiabesity are diverse and severe, encompassing both macrovascular and microvascular complications. Coronary artery disease represents the most common manifestation, with individuals with cardiodiabesity experiencing earlier onset and more aggressive disease progression. The presence of metabolic syndrome increases the risk of developing cardiac dysfunction and heart failure more than 3-fold during 20-year follow-up periods.[5]
Heart failure represents a particularly significant complication in cardiodiabesity, with distinct phenotypic presentations. Heart failure with preserved ejection fraction (HFpEF) is especially common in this population, characterized by diastolic dysfunction, concentric ventricular hypertrophy, and exercise intolerance. Visceral adipose tissue plays a major role in the development, pathophysiology, and adverse outcomes of HFpEF in obese individuals.[10]
Atrial fibrillation occurs with increased frequency in cardiodiabesity patients, related to structural cardiac changes, autonomic dysfunction, and inflammatory processes. The combination of diabetes and cardiovascular disease also increases the risk of sudden cardiac death, particularly in the setting of heart failure and left ventricular dysfunction.[10]
Metabolic and Renal Complications
Cardiodiabesity is associated with accelerated progression of diabetic complications, including nephropathy, retinopathy, and neuropathy. The presence of cardiovascular disease accelerates the development and progression of chronic kidney disease, creating a bidirectional relationship where kidney dysfunction further increases cardiovascular risk.[3]
Non-alcoholic fatty liver disease (NAFLD) is increasingly recognized as both a component and consequence of cardiodiabesity.
The liver serves as a central metabolic organ in this condition, with hepatic insulin resistance contributing to dyslipidemia, glucose intolerance, and systemic inflammation. Progressive NAFLD can lead to cirrhosis and hepatocellular carcinoma, adding additional morbidity and mortality risks.
The metabolic syndrome phenotype is frequently present in cardiodiabesity patients, characterized by central obesity, insulin resistance, dyslipidemia, and hypertension. This clustering of risk factors creates a synergistic effect, with patients having 2-fold increased risk of atherosclerotic cardiovascular diseases and 5-fold increased risk of developing diabetes.[5]
Systemic Inflammatory Consequences
Cardiodiabesity is characterized by chronic systemic inflammation that affects multiple organ systems beyond the cardiovascular system. This inflammatory state contributes to accelerated aging, increased cancer risk, and greater susceptibility to infections and other inflammatory conditions. The pro-inflammatory milieu also impairs wound healing and increases the risk of surgical complications.[6]
Cognitive dysfunction and increased risk of dementia are increasingly recognized complications of cardiodiabesity. The combination of vascular disease, insulin resistance, and chronic inflammation contributes to accelerated cognitive decline and increased risk of Alzheimer disease. This neurological dimension of cardiodiabesity has significant implications for quality of life and functional independence.
Diagnostic Approaches and Biomarkers
Clinical Assessment Framework
The diagnosis of cardiodiabesity requires a comprehensive assessment encompassing clinical history, physical examination, laboratory testing, and imaging studies. The 2023 ESC Guidelines recommend systematic screening for diabetes in all patients with CVD, while all patients with diabetes should be evaluated for cardiovascular disease risk and presence. This bidirectional screening approach is essential given the high prevalence of undetected conditions in each population.[2]
Risk stratification tools have evolved to incorporate cardiodiabesity concepts, with the introduction of diabetes-specific cardiovascular risk calculators such as SCORE2-Diabetes. This tool provides 10-year risk estimates for fatal and non-fatal cardiovascular events specifically in patients with T2DM without established atherosclerotic cardiovascular disease. The calculator serves as a guide for clinical decision-making and treatment intensification.
Physical examination should focus on identifying manifestations of metabolic syndrome, including central obesity (waist circumference >40 inches in men, >35 inches in women), acanthosis nigricans, and signs of insulin resistance. Cardiovascular examination should assess for evidence of heart failure, peripheral arterial disease, and carotid bruits.[11]
Laboratory Biomarkers and Emerging Indicators
Traditional biomarker assessment in cardiodiabesity includes comprehensive metabolic panels encompassing glucose metabolism (HbA1c, fasting glucose, oral glucose tolerance testing), lipid profiles (total cholesterol, LDL, HDL, triglycerides, non-HDL cholesterol), kidney function (creatinine, eGFR, albumin-to-creatinine ratio), and inflammatory markers (C-reactive protein).[12]
Advanced lipid testing provides additional prognostic information, with apolipoprotein B (ApoB) and lipoprotein(a) [Lp(a)] showing superior cardiovascular risk prediction compared to traditional LDL cholesterol measurements. ApoB, as a component of atherogenic lipoproteins, provides better assessment of cardiovascular risk than LDL cholesterol alone. Lp(a) has strong Mendelian randomization evidence for coronary heart disease and is increasingly recognized as an important therapeutic target.[13]
Cardiac biomarkers play crucial roles in cardiodiabesity management. B-type natriuretic peptide (BNP) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) are essential for heart failure diagnosis, risk stratification, and monitoring treatment response. Cardiac troponins (cTnI and cTnT) provide prognostic information beyond clinical markers and are recommended for early risk assessment in patients with suspected cardiovascular complications.[14]
Emerging biomarkers include soluble suppression of tumorigenicity 2 (sST2), which provides prognostic information supplementary to NT-proBNP, and various inflammatory markers that reflect the chronic inflammatory state characteristic of cardiodiabesity. High-sensitivity C-reactive protein (hs-CRP) remains valuable for cardiovascular risk stratification in apparently healthy individuals.[12]
Imaging and Functional Assessment
Coronary artery calcium (CAC) scoring has emerged as a powerful tool for cardiovascular risk assessment in cardiodiabesity patients. CAC represents subclinical coronary atherosclerosis and reflects cumulative lifetime exposure to cardiovascular risk factors. Recent guidelines recommend selective use of CAC scoring for primary prevention decision-making, as incorporating CAC into traditional risk factor models provides statistically and clinically significant enhancement in risk discrimination.[14]
Echocardiographic assessment is essential for detecting cardiac complications of cardiodiabesity, including left ventricular hypertrophy, diastolic dysfunction, and reduced ejection fraction. Advanced echocardiographic techniques such as strain imaging can detect subclinical myocardial dysfunction, with abnormal subclinical myocardial function prevalence ranging from 37% to 54% in obesity.[5]
Exercise stress testing serves dual diagnostic and prognostic purposes in cardiodiabesity patients. Beyond detecting inducible ischemia, exercise capacity provides important prognostic information, with cardiorespiratory fitness being a powerful predictor of cardiovascular outcomes independent of traditional risk factors.[15]
Management Strategies and Therapeutic Interventions
Lifestyle Interventions and Primary Prevention
Comprehensive lifestyle modification remains the cornerstone of cardiodiabesity management, with evidence demonstrating that up to 80% of cardiovascular disease is preventable through lifestyle interventions. The most important behavioral risk factors—unhealthy diet, physical inactivity, tobacco use, and harmful alcohol consumption—are all modifiable through targeted interventions.
Dietary interventions should emphasize evidence-based patterns including the Mediterranean diet, DASH (Dietary Approaches to Stop Hypertension) diet, and healthy plant-based diets. These dietary patterns consistently demonstrate cardiovascular benefits and are characterized by high intake of fruits, vegetables, whole grains, legumes, nuts, and lean proteins, while limiting red meat, processed foods, refined sugars, and saturated fats. A recent meta-analysis of Mediterranean diet studies showed strong evidence for reduced incidence of collective cardiodiabesity risk factors.[1]
Physical activity recommendations include at least 150 minutes per week of moderate-intensity aerobic activity or 75 minutes per week of vigorous-intensity activity, along with muscle-strengthening activities at least twice weekly. Regular physical activity provides benefits across all components of cardiodiabesity, improving insulin sensitivity, blood pressure, lipid profiles, and cardiovascular fitness.[16]
Weight management strategies should target sustained weight loss through combination approaches including dietary modification, physical activity, behavioral counseling, and when appropriate, pharmacotherapy or bariatric surgery. Even modest weight loss of 3-5% provides clinically meaningful benefits for triglycerides, blood glucose, and diabetes risk.[17]
Pharmacological Management
Antidiabetic Medications with Cardiovascular Benefits
The landscape of diabetes management has been revolutionized by glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and sodium-glucose cotransporter 2 (SGLT2) inhibitors, both of which provide significant cardiovascular benefits beyond glycemic control. Current guidelines strongly recommend these agents for patients with diabetes and established cardiovascular disease or high cardiovascular risk, independent of baseline HbA1c levels.[2]
GLP-1 receptor agonists have demonstrated significant reductions in major adverse cardiovascular events (MACE), with meta-analyses showing risk reduction of approximately 12-21%. These agents are particularly effective in reducing stroke and myocardial infarction risk. The cardiovascular benefits appear to be mediated through multiple mechanisms including weight loss, blood pressure reduction, improved lipid profiles, and direct cardioprotective effects. Recent studies suggest that tirzepatide, a dual GLP-1/GIP receptor agonist, may provide superior cardiovascular and kidney benefits compared to traditional GLP-1 RAs.[18]
SGLT2 inhibitors provide complementary cardiovascular benefits, with particular efficacy in reducing heart failure hospitalizations and cardiovascular death. Three major cardiovascular outcome trials have demonstrated significant reductions in cardiovascular events, with benefits extending to primary prevention populations. The heart failure benefits of SGLT2 inhibitors have been consistently demonstrated across the spectrum of ejection fractions.[19]
Cardiovascular Risk Reduction Therapies
Lipid management requires intensive approaches in cardiodiabesity patients, with high-intensity statin therapy as the preferred initial treatment. The goal is to achieve LDL cholesterol reductions of ≥50% and target levels appropriate for risk category. When maximally tolerated statin therapy is insufficient, combination therapy with ezetimibe and PCSK9 monoclonal antibodies provides additional cardiovascular risk reduction.[20]
Blood pressure management follows intensive targets, with current guidelines recommending blood pressure <130/80 mmHg for most patients with diabetes and cardiovascular disease. First-line agents include ACE inhibitors or ARBs, thiazide or thiazide-like diuretics, and calcium channel blockers. The choice of specific agents should consider comorbidities and individual patient factors.[21]
Antiplatelet therapy with aspirin is recommended for secondary prevention in patients with established atherosclerotic cardiovascular disease. The 2023 ESC Guidelines provide detailed recommendations for antithrombotic therapy in various clinical scenarios, including dual antiplatelet therapy duration and triple therapy considerations.[2]
Emerging Therapeutic Approaches
Weight Management Pharmacotherapy
Recent advances in obesity pharmacotherapy have provided new options for cardiodiabesity management. Semaglutide and tirzepatide have demonstrated superior efficacy compared to traditional weight loss medications, achieving weight reductions of 15-20% in clinical trials. The American College of Cardiology has issued guidance recommending consideration of these medications as first-line treatment for eligible patients, rather than requiring failure of lifestyle interventions first.[17]
These medications provide cardiovascular benefits beyond weight loss, including reductions in major adverse cardiovascular events, particularly in individuals with type 2 diabetes and elevated cardiovascular risk. Clinical trial and real-world data support their use for both weight management and cardiovascular risk reduction.[17]
Multidisciplinary Care Models
Team-based approaches are essential for optimal cardiodiabesity management. Coordinated care models should include primary care physicians, cardiologists, endocrinologists, dietitians, exercise physiologists, and behavioral health specialists. This multidisciplinary approach is crucial for addressing the complex, multifaceted nature of cardiodiabesity.[2]
Person-centered care approaches emphasize shared decision-making, cultural competency, and addressing social determinants of health. The 2023 ESC Guidelines specifically recommend person-centered care strategies that account for individual patient preferences, cultural backgrounds, and social circumstances.[2]
Economic Impact and Healthcare Utilization
Cost Burden Analysis
The economic impact of cardiodiabesity represents one of the most significant healthcare cost drivers in modern medicine, with estimated annual costs of $838 billion in the United States. This massive economic burden encompasses both direct healthcare costs and indirect costs related to lost productivity, disability, and premature mortality. Individual component costs include approximately $173 billion annually for obesity, $219 billion for heart disease and stroke, and $327 billion for diabetes (including both healthcare expenses and lost productivity).[8]
Chronic conditions drive 90% of the country’s $4.1 trillion annual healthcare expenditure, with cardiodiabesity representing a substantial portion of this burden. The progressive nature of cardiodiabesity significantly amplifies costs as patients advance through disease stages, with healthcare utilization and costs increasing dramatically with disease progression.[22]
Analysis of healthcare utilization patterns reveals that average total cost of care increases significantly among those who progress from one disease phase to the next. This progressive cost escalation highlights the economic importance of early intervention and prevention strategies to halt or slow disease progression. The cost-effectiveness of prevention interventions becomes particularly compelling when considering the exponential cost increases associated with advanced cardiodiabesity complications.[9]
Healthcare Resource Utilization Patterns
Healthcare service utilization varies significantly across cardiodiabesity disease stages. Early-stage cardiodiabesity patients primarily utilize outpatient services for risk factor management and preventive care. Active-stage patients require more intensive management with increased specialty care, diagnostic testing, and medication management. Advanced-stage patients demonstrate the highest healthcare utilization with frequent hospitalizations, emergency department visits, and complex interventions.[22]
Hospitalization patterns show that cardiodiabesity patients experience longer length of stay, higher readmission rates, and increased intensive care unit utilization compared to patients without cardiodiabesity. Heart failure hospitalizations represent a particularly significant cost driver, with SGLT2 inhibitors and other evidence-based therapies demonstrating cost-effectiveness through reduction in heart failure hospitalizations.[2]
The medication cost component of cardiodiabesity management has grown significantly with the introduction of newer therapeutic agents. While newer medications such as GLP-1 receptor agonists and SGLT2 inhibitors are associated with higher upfront costs, economic analyses demonstrate their cost-effectiveness through reduction in cardiovascular events and hospitalizations.[4]
Economic Benefits of Prevention and Treatment
Prevention strategies offer substantial economic benefits through avoidance of expensive complications and hospitalizations. Studies demonstrate that implementing programs to prevent and control cardiodiabesity conditions can provide significant return on investment through reduced healthcare utilization and improved productivity. The key to achieving these economic benefits is early identification and intervention before progression to advanced disease stages.[22]
Evidence-based therapies such as GLP-1 receptor agonists and SGLT2 inhibitors demonstrate favorable cost-effectiveness profiles despite higher upfront medication costs. Economic analyses consistently show that the costs of these medications are offset by reductions in cardiovascular events, hospitalizations, and long-term complications. The cost-effectiveness becomes even more favorable when considering quality-adjusted life-years gained.[18]
Multidisciplinary care models have demonstrated both clinical effectiveness and cost-effectiveness for cardiodiabesity management. These models reduce healthcare utilization through better care coordination, reduced duplication of services, and improved medication adherence. The upfront investment in care coordination and patient education pays dividends through reduced emergency department visits and hospitalizations.[17]
Prevention Strategies and Public Health Approaches
Primary Prevention Frameworks
Population-level prevention strategies for cardiodiabesity require comprehensive approaches addressing environmental, policy, and individual factors. The World Health Organization emphasizes that addressing behavioral risk factors through policy interventions is essential for population-wide prevention. Key policy interventions include tobacco control measures, food labeling requirements, restrictions on marketing of unhealthy foods, and urban planning initiatives that promote physical activity.[23]
Environmental modifications play crucial roles in cardiodiabesity prevention. Creating environments where healthy choices are available, affordable, and accessible requires coordinated efforts across multiple sectors including agriculture, transportation, urban planning, and healthcare. Examples include ensuring access to healthy foods in underserved areas, creating safe spaces for physical activity, improving air quality, and implementing policies that reduce exposure to cardiovascular risk factors.[24]
Healthcare system initiatives should focus on early identification and intervention. This includes systematic screening programs for cardiovascular risk factors, diabetes prevention programs, and weight management services. The effectiveness of these programs is enhanced when they address social determinants of health and provide culturally appropriate interventions.[2]
Secondary Prevention and Risk Factor Modification
Intensive risk factor modification in patients with established cardiodiabesity can significantly slow disease progression and reduce complications. The 2023 ESC Guidelines emphasize multifactorial approaches targeting all modifiable risk factors simultaneously. This includes aggressive lipid lowering, blood pressure control, glycemic management, antiplatelet therapy, and lifestyle interventions.[2]
Medication adherence represents a critical component of secondary prevention, with studies showing that poor adherence to evidence-based therapies significantly increases cardiovascular risk. Healthcare systems should implement strategies to improve medication adherence including patient education, simplified dosing regimens, medication synchronization programs, and addressing cost barriers.[2]
Regular monitoring and follow-up are essential for successful secondary prevention. This includes routine assessment of cardiovascular risk factors, medication effectiveness and tolerability, and early detection of complications. The frequency and intensity of monitoring should be individualized based on disease severity and risk factors.[2]
Community-Based Prevention Programs
Community health initiatives have demonstrated effectiveness in preventing cardiodiabesity through population-wide interventions. Successful programs include community gardens, walking programs, health screenings in community settings, and partnerships with faith-based organizations and community centers. These programs are particularly effective when they address cultural factors and social determinants of health.[16]
Worksite wellness programs offer opportunities to reach large populations with prevention interventions. Evidence-based worksite programs include health risk assessments, biometric screenings, lifestyle modification programs, and environmental modifications in workplace settings. The analysis showing that 40% of households have a primary member with cardiodiabesity underscores the importance of workplace interventions.[8]
School-based interventions provide opportunities for primary prevention in children and adolescents. These programs should focus on establishing healthy dietary patterns, promoting physical activity, preventing tobacco use, and providing health education. Early intervention in childhood and adolescence may prevent the development of risk factors that lead to adult cardiodiabesity.[24]
Future Directions and Emerging Research
Precision Medicine Approaches
Genomic medicine is poised to revolutionize cardiodiabesity management through identification of genetic variants that influence disease risk, treatment response, and prognosis. Mendelian randomization studies have provided strong evidence for causal relationships between various biomarkers and cardiovascular outcomes, informing therapeutic target identification. Future research should focus on developing polygenic risk scores that can improve risk prediction beyond traditional clinical factors.[13]
Pharmacogenomics research is investigating genetic factors that influence medication effectiveness and adverse effects in cardiodiabesity patients. This includes studies of genetic variants affecting response to statins, antihypertensive medications, and diabetes medications. Personalized medicine approaches based on genetic testing may optimize medication selection and dosing.[2]
Biomarker-guided therapy represents an emerging approach to optimize cardiodiabesity management. Research is focusing on identifying biomarkers that can guide treatment decisions, monitor treatment response, and predict complications. This includes investigation of novel biomarkers such as microRNAs, metabolomics profiles, and inflammatory markers that may provide superior risk stratification compared to traditional markers.[12]
Technological Innovations
Digital health technologies offer promising approaches for cardiodiabesity prevention and management. This includes mobile health applications, wearable devices, telemedicine platforms, and remote monitoring systems. These technologies can provide continuous monitoring of risk factors, deliver personalized interventions, and improve access to care particularly in underserved populations.[17]
Artificial intelligence and machine learning applications are being developed to improve risk prediction, optimize treatment selection, and identify patients at highest risk for complications. These technologies can analyze large datasets to identify patterns and relationships that may not be apparent through traditional statistical approaches. Future applications may include AI-guided treatment optimization and predictive modeling for disease progression.[25]
Continuous glucose monitoring and other continuous monitoring technologies provide opportunities for real-time management of cardiodiabesity risk factors. These technologies can provide detailed information about glucose patterns, physical activity levels, and other physiological parameters that inform treatment decisions. Integration of multiple monitoring technologies may provide comprehensive assessment of cardiodiabesity status and treatment response.[2]
Novel Therapeutic Targets
Inflammatory pathway modulation represents a promising therapeutic approach given the central role of inflammation in cardiodiabesity pathophysiology. Research is investigating anti-inflammatory therapies specifically for cardiometabolic conditions, including interleukin inhibitors and other targeted anti-inflammatory approaches. The challenge is identifying interventions that reduce pathological inflammation without compromising immune function.[6]
Metabolic pathway targeting includes investigation of novel approaches to improve insulin sensitivity, enhance fat oxidation, and optimize metabolic substrate utilization. This includes research on mitochondrial function enhancement, adipokine modulation, and targeting specific metabolic enzymes. These approaches may provide more targeted interventions compared to current broad-spectrum approaches.[26]
Gut microbiome interventions are emerging as potential therapeutic targets for cardiodiabesity. Research demonstrates that gut microbiome composition influences metabolism, inflammation, and cardiovascular risk. Therapeutic approaches under investigation include probiotics, prebiotics, fecal microbiota transplantation, and microbiome-targeted medications. These interventions may provide novel approaches to modify cardiodiabesity risk factors.[6]
Conclusion
Cardiodiabesity represents a complex, multifaceted health challenge that demands comprehensive, coordinated approaches spanning clinical medicine, public health, and healthcare policy. The recognition that cardiovascular disease, type 2 diabetes, and obesity are interconnected conditions sharing common pathophysiological mechanisms has transformed our understanding of chronic disease management and prevention strategies. With over 4.9 million Americans affected by various stages of cardiodiabesity and an annual economic burden approaching $838 billion, this condition represents one of the most significant health crises of our time.[1]
The three-stage progression model of cardiodiabesity provides a valuable framework for understanding disease evolution and targeting interventions. The finding that 27.4% of patients with early-stage risk factors progress to active disease within one year, and 88.4% of those with active cardiodiabesity develop complications, underscores both the progressive nature of the condition and the critical importance of early identification and intervention. This rapid progression timeline creates both urgency for action and opportunities for prevention that can dramatically alter disease trajectories.[3]
Evidence-based management strategies have evolved significantly with the introduction of novel therapeutic agents that provide benefits beyond traditional risk factor modification. GLP-1 receptor agonists and SGLT2 inhibitors represent paradigm-shifting therapies that address multiple components of cardiodiabesity simultaneously, providing cardiovascular benefits, weight management, and glycemic control in single interventions. The emerging recognition that these medications should be considered first-line therapies rather than last-resort options reflects the evolution toward more proactive, comprehensive management approaches.[2]
Prevention strategies offer the greatest potential for reducing the burden of cardiodiabesity, with evidence demonstrating that up to 80% of cardiovascular disease is preventable through lifestyle interventions and risk factor modification. However, successful prevention requires coordinated efforts addressing individual behaviors, environmental factors, and systemic barriers to healthy living. The finding that cardiodiabesity clusters within households suggests that family-based and community-based interventions may be particularly effective.[8]
Future directions in cardiodiabesity research and management hold promise for more personalized, effective approaches. Precision medicine applications incorporating genetic factors, biomarker-guided therapy, and digital health technologies may optimize treatment selection and monitoring. The integration of artificial intelligence and machine learning approaches may enhance risk prediction and treatment optimization beyond current capabilities.[12]
The economic imperative for addressing cardiodiabesity cannot be overstated. The exponential increase in healthcare costs associated with disease progression from early-stage risk factors to advanced complications demonstrates that prevention and early intervention strategies offer substantial return on investment. Healthcare systems, employers, and policymakers must recognize that investment in cardiodiabesity prevention and management represents not only a moral imperative but also an economic necessity.[22]
Moving forward, success in addressing the cardiodiabesity epidemic will require coordinated efforts across multiple sectors including healthcare, public health, policy, education, and community organizations. The complexity of cardiodiabesity demands equally complex solutions that address root causes while providing effective treatment for those already affected. The tools and knowledge exist to make significant progress against this condition; what remains is the commitment to implement evidence-based strategies at the scale required to match the magnitude of the challenge.
References
- Mediterranean Diet and Cardiodiabesity: A Review. https://pmc.ncbi.nlm.nih.gov/articles/PMC4179172/ Accessed November 3, 2025
- Just a moment.... https://academic.oup.com/eurheartj/article/44/39/4043/7238227 Accessed November 3, 2025
- Cardiodiabesity: Epidemiology, resource and economic impact. https://pmc.ncbi.nlm.nih.gov/articles/PMC11582466/ Accessed November 3, 2025
- Cardiodiabesity Health Care Trends and Solutions. https://www.evernorth.com/articles/three-biggest-drivers-health-care-costs Accessed November 3, 2025
- Cardiovascular Consequences of Metabolic Syndrome. https://pmc.ncbi.nlm.nih.gov/articles/PMC5393930/ Accessed November 3, 2025
- Molecular Mechanisms of Obesity-Linked Cardiac Dysfunction: An Up-Date on Current Knowledge. https://pmc.ncbi.nlm.nih.gov/articles/PMC8000147/ Accessed November 3, 2025
- https://www.heart.org/-/media/PHD-Files-2/Science-News/2/2024-Heart-and-Stroke-Stat-Update/2024-Statistics-At-A-Glance-final_2024.pdf. https://www.heart.org/-/media/PHD-Files-2/Science-News/2/2024-Heart-and-Stroke-Stat-Update/2024-Statistics-At-A-Glance-final_2024.pdf Accessed November 3, 2025
- Research: Addressing cardiodiabesity at the household level could lower cost trend. https://www.evernorth.com/articles/research-addressing-cardiodiabesity-household-level-could-lower-cost-trend Accessed November 3, 2025
- Cardiodiabesity: Epidemiology, resource and economic impact. https://pubmed.ncbi.nlm.nih.gov/39583639/ Accessed November 3, 2025
- Just a moment.... https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.120.316101 Accessed November 3, 2025
- Heart disease prevention: Strategies to keep your heart healthy. https://www.mayoclinic.org/diseases-conditions/heart-disease/in-depth/heart-disease-prevention/art-20046502 Accessed November 3, 2025
- Just a moment.... https://spj.science.org/doi/10.34133/jbioxresearch.0030 Accessed November 3, 2025
- Just a moment.... https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.123.322000 Accessed November 3, 2025
- Unveiling the Role of Biomarkers in Cardiovascular Risk Assessment and Prognosis. https://pmc.ncbi.nlm.nih.gov/articles/PMC10849159/ Accessed November 3, 2025
- Just a moment.... https://www.ahajournals.org/doi/10.1161/circulationaha.104.482570 Accessed November 3, 2025
- Lifestyle Strategies for Risk Factor Reduction, Prevention, and Treatment of Cardiovascular Disease. https://pmc.ncbi.nlm.nih.gov/articles/PMC6378495/ Accessed November 3, 2025
- American College of Cardiology Issues Guidance on Weight Management Drugs. https://www.acc.org/About-ACC/Press-Releases/2025/06/20/14/11/American-College-of-Cardiology-Issues-Guidance-on-Weight-Management-Drugs Accessed November 3, 2025
- Long-Term Cardiovascular Outcomes of Glucagon-Like Peptide-1 (GLP-1) Receptor Agonists in Type 2 Diabetes: A Systematic Review. https://pubmed.ncbi.nlm.nih.gov/39568487/ Accessed November 3, 2025
- Just a moment.... https://www.ahajournals.org/doi/10.1161/cir.0000000000000678 Accessed November 3, 2025
- Just a moment.... https://www.ahajournals.org/doi/10.1161/CIR.0000000000001168 Accessed November 3, 2025
- Management of Cardiovascular and Diabetes Risks Based on National Guidelines - StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK580534/ Accessed November 3, 2025
- Study: Progression of cardiodiabesity increases care utilization and costs. https://www.evernorth.com/articles/study-progression-cardiodiabesity-increases-care-utilization-and-costs Accessed November 3, 2025
- CVD Prevention | What We Do. https://world-heart-federation.org/what-we-do/prevention/ Accessed November 3, 2025
- Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) Accessed November 3, 2025
- Biomarker identification and risk assessment of cardiovascular disease based on untargeted metabolomics and machine learning. https://www.nature.com/articles/s41598-024-77352-3 Accessed November 3, 2025
- Pathophysiology of Cardiovascular Complications in Obesity and Diabetes. https://lupinepublishers.com/diabetes-obesity-journal/fulltext/pathophysiology%20of%20cardiovascular%20complications%20in%20obesity%20and%20diabetes.ID.000163.php Accessed November 3, 2025
