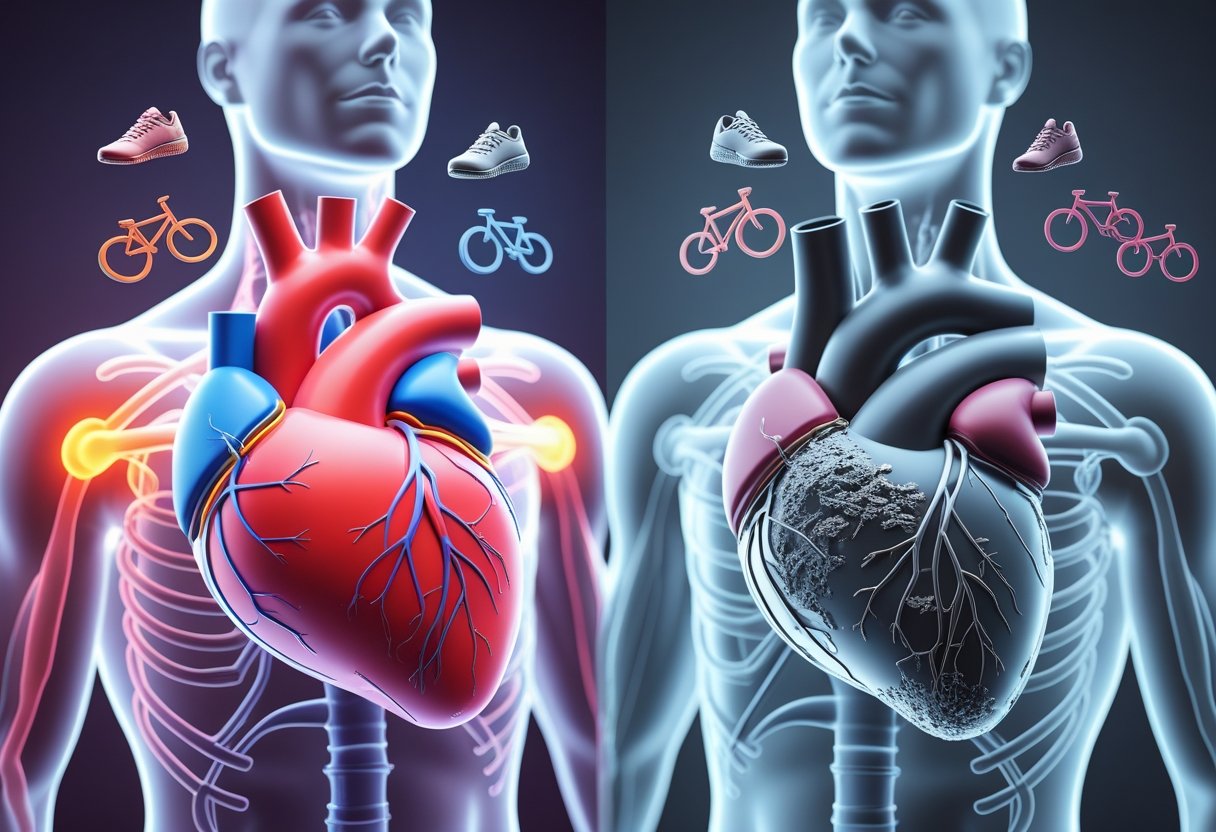
When people don’t follow recommended exercise guidelines, their heart disease risk increases significantly. Missing regular physical activity leads to weakened heart muscle, higher blood pressure, poor cholesterol levels, and increased inflammation throughout the body.
Physical inactivity has been identified as the fourth leading risk factor for death worldwide, causing approximately 3.2 million deaths each year. The body responds to exercise gaps by losing cardiovascular fitness within just weeks, while beneficial changes like improved blood flow and reduced arterial stiffness begin to reverse.
The good news is that even short bouts of activity lasting just a few minutes can help reduce heart disease risk. Understanding what happens during exercise lapses helps people make better choices about getting back on track with their fitness routines.
Key Takeaways
- Missing exercise guidelines weakens the heart and increases blood pressure, cholesterol problems, and body-wide inflammation
- The body loses heart-protective benefits within weeks of stopping regular physical activity, but improvements can return quickly when exercise resumes
- Even brief periods of daily movement count toward reducing heart disease risk and preventing long-term cardiovascular problems
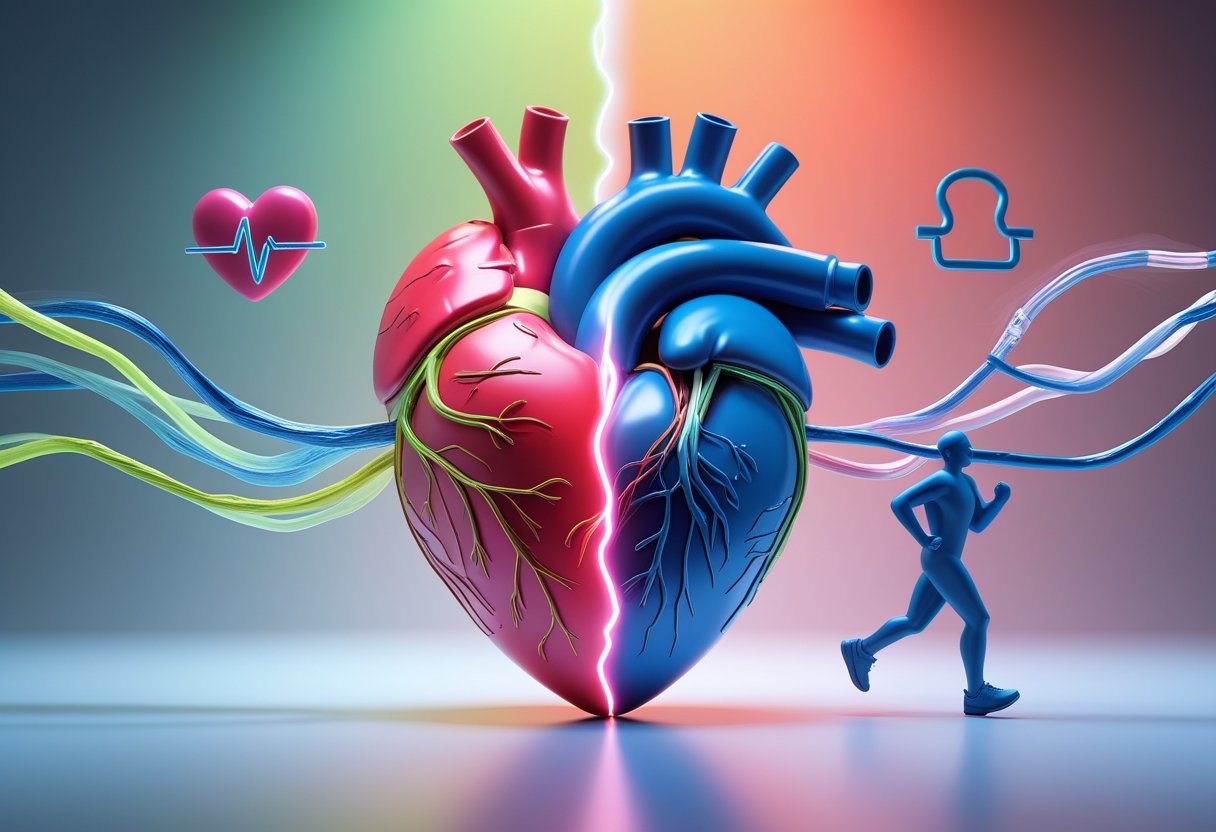
How Exercise Influences Heart Disease Risk

Regular physical activity creates powerful changes in the cardiovascular system that directly reduce heart disease risk. Exercise strengthens the heart muscle, improves blood flow, and helps control key risk factors like blood pressure and cholesterol levels.
Impact of Physical Activity on Cardiovascular Health
Physical activity strengthens your heart muscle when done regularly. A stronger heart pumps blood more efficiently throughout the body.
The heart becomes better at delivering oxygen-rich blood to muscles and organs. This improved pumping ability reduces the workload on the cardiovascular system during daily activities.
Exercise helps control major heart disease risk factors including:
- High blood pressure – Regular activity lowers both systolic and diastolic readings
- Bad cholesterol – Physical activity reduces LDL cholesterol that clogs arteries
- Triglycerides – Exercise decreases these harmful blood fats
- Blood sugar – Activity helps muscles use glucose more effectively
People who remain inactive face significantly higher heart disease risk. Studies show that physical inactivity ranks as a major risk factor alongside smoking and high cholesterol.
Mechanisms Behind Exercise Benefits
Exercise triggers specific changes in blood vessels that protect against heart disease. Physical activity widens capillaries throughout the body, improving oxygen delivery to tissues.
Regular activity reduces inflammation markers in the blood. Lower inflammation levels decrease the risk of plaque buildup in coronary arteries.
Exercise improves cholesterol profiles by raising HDL (good) cholesterol while lowering harmful LDL cholesterol. This balance helps prevent arterial blockages.
Physical activity enhances insulin sensitivity. Better blood sugar control reduces diabetes risk, which is a major contributor to heart disease.
The heart muscle adapts to regular exercise by becoming more efficient. This adaptation allows the heart to pump the same amount of blood with fewer beats, reducing overall cardiovascular stress.
Role of Muscle Strength and Flexibility in Heart Protection
Muscle strength training provides unique cardiovascular benefits beyond aerobic exercise. Strong muscles require less effort during daily activities, reducing strain on the heart.
Resistance exercises help maintain healthy blood pressure levels. Stronger muscles also improve glucose metabolism, supporting better blood sugar control.
Flexibility training through stretching or yoga supports heart health indirectly. Better flexibility reduces injury risk, allowing people to maintain consistent exercise routines.
Key muscle strength benefits for heart health:
- Improved blood pressure regulation
- Better insulin sensitivity
- Enhanced metabolism
- Reduced cardiovascular workload during activities
Combining muscle strength, flexibility, and aerobic exercise creates the most comprehensive heart protection. Each type of physical activity contributes different mechanisms that work together to reduce heart disease risk.
What Happens When You Don’t Meet Exercise Guidelines
Missing regular exercise creates measurable changes in cardiovascular health within weeks. Inactive people are nearly twice as likely to develop heart disease compared to those who stay active.
Increased Heart Disease Risk Factors
Blood pressure begins to rise when people stop exercising regularly. The heart loses its ability to pump blood efficiently without consistent physical activity.
Cholesterol levels shift in dangerous directions. HDL (good) cholesterol drops while LDL (bad) cholesterol increases.
Blood sugar control becomes harder without exercise. Muscles rely on physical activity to absorb glucose effectively from the bloodstream.
A sedentary lifestyle can have detrimental effects on heart health, leading to complications that increase cardiovascular disease risk. These changes happen even in people with no other risk factors.
The combination of these factors creates a compound effect. Each risk factor makes the others worse over time.
Potential for Deterioration of Heart Function
The heart muscle weakens without regular exercise. Like any muscle, it needs consistent work to stay strong and efficient.
Heart rate variability decreases in inactive people. This means the heart becomes less adaptable to different demands throughout the day.
Stroke volume drops when exercise stops. The heart pumps less blood with each beat, forcing it to work harder during daily activities.
Circulation becomes less effective without physical activity. Blood flow to organs and tissues reduces, affecting overall health.
Recovery time after physical exertion increases. Simple activities like climbing stairs become more challenging as heart function declines.
Risk of Weight Gain and Metabolic Issues
Weight gain accelerates when exercise stops. The body burns fewer calories while muscle mass decreases and fat storage increases.
Metabolism slows down without regular physical activity. This makes it easier to gain weight and harder to lose it later.
Insulin resistance develops more quickly in inactive people. Cells become less responsive to insulin, raising blood sugar levels.
Inflammation markers increase in the blood. This chronic low-grade inflammation damages blood vessels and heart tissue over time.
Sleep quality often worsens without exercise. Poor sleep further disrupts metabolism and increases stress hormones that affect heart health.
Evidence-Based Exercise Guidelines for Heart Health
The American Heart Association and federal health guidelines provide clear targets for physical activity that can significantly reduce heart disease risk. These recommendations focus on specific amounts of weekly exercise, appropriate intensity levels, and the most effective types of activities for cardiovascular protection.
Recommended Frequency and Duration
Adults need at least 150 minutes per week of moderate-intensity aerobic activity to maintain heart health. This breaks down to about 30 minutes on five days each week.
People can also choose 75 minutes of vigorous exercise weekly instead. This option works well for those with busy schedules who prefer shorter, more intense sessions.
Additional Benefits with More Activity:
- 300 minutes weekly provides even greater heart protection
- Muscle-strengthening exercises should happen at least twice per week
- Even a few minutes of movement counts toward the weekly goal
Breaking up exercise throughout the day works just as well as longer sessions. Three 10-minute walks provide the same benefits as one 30-minute walk.
Intensity: How Hard Should You Work?
Moderate intensity means a person can still talk while exercising but will breathe harder than normal. Their heart rate increases but they won’t get out of breath from conversation.
Moderate-Intensity Activities:
- Brisk walking at 2.5+ mph
- Dancing
- Water aerobics
- Gardening
- Doubles tennis
Vigorous intensity pushes the body further. People will sweat and find it hard to talk without getting breathless.
Vigorous-Intensity Activities:
- Running
- Swimming laps
- Singles tennis
- Cycling over 10 mph
- Jumping rope
The best approach combines both intensity levels throughout the week. This provides maximum heart protection and prevents workout boredom.
Choosing the Right Types of Activity
Aerobic exercise provides the biggest heart benefits by strengthening the cardiovascular system. Walking programs offer the simplest starting point since they’re free and can be done anywhere.
Best Aerobic Options:
- Walking (easiest for beginners)
- Swimming (gentle on joints)
- Cycling
- Dancing
- Hiking
Swimming works especially well for people with joint problems or injuries. The water supports body weight while providing excellent cardiovascular exercise.
Strength training should complement aerobic exercise at least twice weekly. This combination helps control multiple risk factors for heart disease including blood pressure and diabetes risk.
People with existing heart conditions should talk with their doctor before starting any new physical activity program.
Consequences of Missing Fitness Recommendations
When people fail to meet exercise guidelines, their cardiovascular system faces immediate and long-term challenges. The heart muscle weakens while blood vessels lose their ability to adapt to physical demands.
Loss of Muscle Strength and Flexibility
Physical inactivity leads to cardiovascular disease as the heart muscle itself begins to weaken. The heart is a muscle that needs regular activity to stay strong and efficient.
Without enough exercise, the heart loses its ability to pump blood effectively. This makes everyday tasks feel harder and more tiring.
Key Changes in Heart Function:
- Reduced stroke volume (less blood pumped per beat)
- Higher resting heart rate
- Decreased cardiac output
- Poor circulation to extremities
Blood vessels also become less flexible when people don’t exercise regularly. The arteries stiffen and cannot expand properly when blood flows through them.
This stiffness forces the heart to work harder to push blood through the body. Over time, this extra work can damage the heart muscle and lead to serious problems.
Heightened Risk of Angina and Chest Pain
People who miss fitness guidelines face a much higher chance of developing chest pain and angina. A sedentary lifestyle can have detrimental effects on heart health by reducing the heart’s ability to handle stress.
Angina happens when the heart muscle doesn’t get enough oxygen-rich blood. This often occurs during physical activity or emotional stress.
Warning Signs Include:
- Chest pressure or squeezing
- Pain in arms, neck, or jaw
- Shortness of breath
- Fatigue during light activity
Without regular exercise, the coronary arteries that feed the heart muscle become narrow and blocked. This makes it harder for blood to reach the heart when it needs more oxygen.
The risk becomes even higher because inactive people often have other heart disease risk factors. These include high blood pressure, diabetes, and excess weight around the waist.
Creating a Safe Exercise Program After Lapses
Getting back into exercise after missing workouts requires a careful approach that prioritizes safety and gradual progress. Healthcare professionals play a key role in designing programs that include proper warm-up, cool-down, and stretching routines.
Strategies for Restarting Physical Activity
People with heart disease should start slowly when returning to exercise after a break. Walking programs offer an excellent starting point for those who have been inactive.
A structured restart plan begins with short sessions every other day. Week one should focus on 10-minute walks at an easy pace. Week two can add a 5-minute warm-up and cool-down period.
By week three, individuals can increase frequency to four times per week. The training period extends to 15 minutes at a slightly faster pace. Week four builds to 20-minute sessions with consistent warm-up and cool-down periods.
Progressive Timeline:
- Weeks 1-2: Every other day, 10-minute sessions
- Weeks 3-4: Four times weekly, 15-20 minutes
- Weeks 5-6: Five days weekly, 25-30 minutes
People should listen to their bodies throughout this process. Normal feelings during exercise include slight tiredness and awareness of breathing. Chest pain, dizziness, or severe shortness of breath are warning signs to stop immediately.
Importance of Warm Up, Cool Down, and Stretching
Proper warm-up prepares the heart for increased activity gradually. A 5-10 minute easy walk before exercising helps blood flow increase slowly. This reduces stress on the cardiovascular system.
Cool-down periods prevent sudden drops in heart rate and blood pressure. Walking slowly for 5 minutes after exercise helps the body transition back to rest. This prevents dizziness and irregular heartbeats.
Essential Components:
- Warm-up: 5-10 minutes of light activity
- Cool-down: 5 minutes of gradual slowing
- Stretching: Focus on major muscle groups
Stretching maintains flexibility and prevents muscle stiffness. It should occur after the cool-down period when muscles are warm. Hold each stretch for 15-30 seconds without bouncing.
The American Heart Association recommends incorporating stretching exercises along with aerobic and strength activities. This combination provides the most benefit for heart health.
Role of Healthcare Professionals in Recovery
A cardiologist should evaluate heart function before any exercise program begins. Many people with heart disease qualify for cardiac rehabilitation, which includes supervised exercise testing.
The cardiac rehabilitation team typically includes multiple specialists. A cardiologist oversees medical care while exercise professionals design safe activity programs. Dietitians provide nutrition guidance for heart health.
Rehabilitation Team Members:
- Cardiologist for medical oversight
- Exercise professional for program design
- Dietitian for nutritional support
- Psychologist for emotional support
A psychologist helps address fears about physical activity after heart problems. Many people feel anxious about exercising after a cardiac event. Professional counseling can overcome these mental barriers.
Working with healthcare professionals ensures safe progression based on individual heart conditions. They monitor responses to increased activity and adjust programs as needed. This professional guidance reduces the risk of complications during exercise recovery.
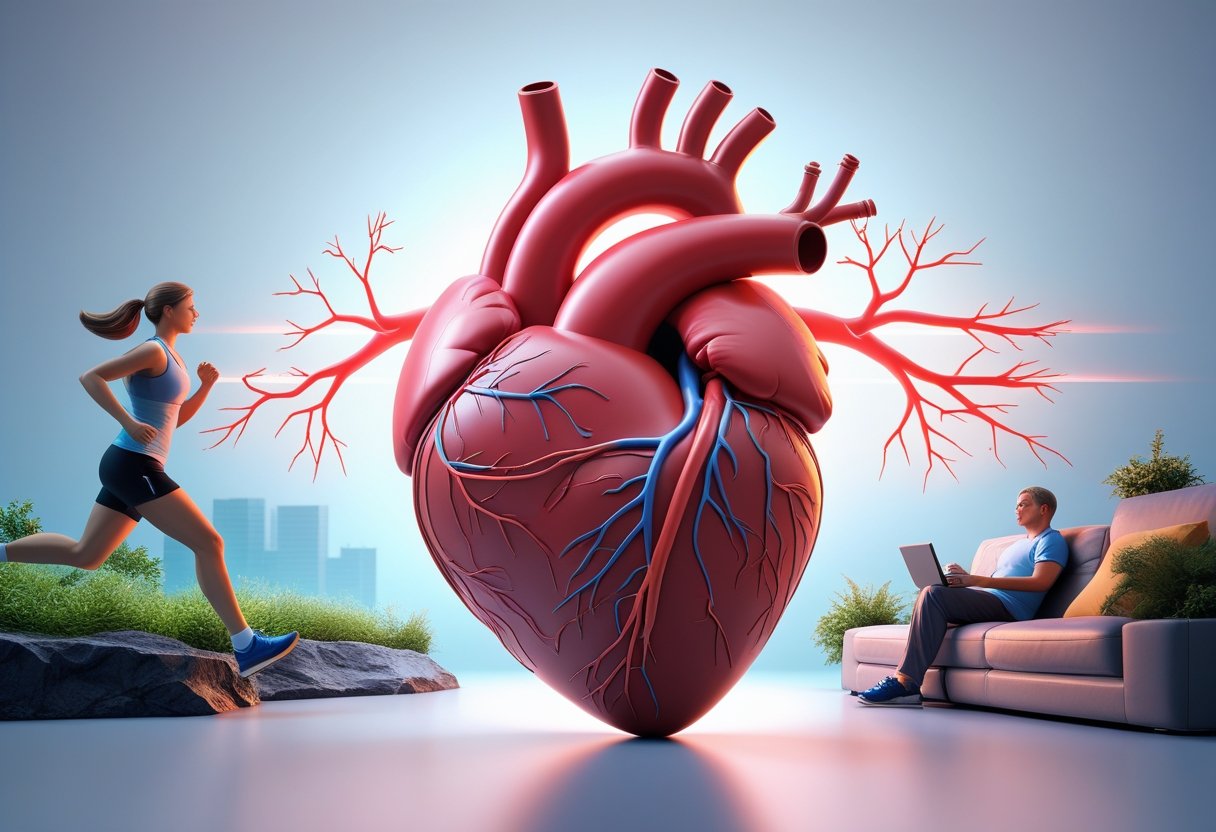
Long-Term Prevention and Maintenance
Successful heart disease prevention requires consistent tracking methods and adaptable exercise choices that people can maintain for years. The key lies in finding sustainable activities and monitoring systems that work with changing life circumstances.
Tracking Progress and Staying Motivated
Regular monitoring helps people stay committed to their exercise goals. Simple tracking methods work better than complex systems for most people.
Daily Activity Logs can include steps taken, minutes exercised, or activities completed. Many people find success with smartphone apps or basic paper calendars.
Weekly Check-ins help identify patterns and problems early. People should note:
- Days missed and reasons why
- Energy levels before and after exercise
- Physical improvements like easier breathing or less fatigue
Monthly Assessments provide bigger picture views. Measuring resting heart rate, blood pressure, or how long it takes to walk a certain distance shows real progress.
Setting small, specific goals maintains motivation better than vague plans. Instead of “exercise more,” people benefit from goals like “walk 20 minutes on Tuesday, Thursday, and Saturday.”
Accountability partners increase success rates significantly. Exercise programs with social support show better long-term results than solo efforts.
Celebrating small wins matters more than waiting for major changes. Completing one week of planned activities deserves recognition.
Adapting Activities: Walking, Swimming, and Beyond
Different life stages and physical changes require flexible exercise approaches. The best program adapts to injuries, aging, weather, and schedule changes.
Walking programs offer the most adaptable foundation. People can start with 10-minute walks and gradually increase time or distance. Indoor malls, treadmills, and neighborhood routes provide year-round options.
Walking intensity can vary from gentle strolls to brisk pace intervals. Those with joint problems benefit from softer surfaces like tracks or grass.
Swimming provides excellent heart benefits with minimal joint stress. Many pools offer water walking classes for beginners or those with mobility limits.
Pool exercises work well for people who cannot do land-based activities. Water supports body weight while providing natural resistance.
Alternative activities prevent boredom and work around limitations:
- Dancing for those who enjoy music and social interaction
- Cycling for people with knee problems who cannot run
- Gardening for gentle, purposeful movement
- Strength training with resistance bands for home workouts
Seasonal adaptations keep programs consistent year-round. Winter indoor options might include mall walking or home videos. Summer heat may require early morning or evening outdoor activities.
Heart-healthy exercise programs should include both cardiovascular activities and strength training elements when possible.
Frequently Asked Questions
Missing exercise guidelines significantly increases heart disease risk through multiple pathways. Regular physical activity requirements vary by age, and specific exercise types provide different cardiovascular benefits.
How does lack of exercise impact the likelihood of developing heart disease?
Physical inactivity directly increases the risk of cardiovascular disease, high blood pressure, and type 2 diabetes. Not being physically active is a risk factor for health problems that can lead to serious complications.
A sedentary lifestyle weakens the heart muscle over time. Regular exercise keeps heart strong, efficient, and resilient, while lack of activity has harmful effects on heart health.
The heart becomes less efficient at pumping blood when exercise is absent. This leads to poor circulation and increases the workload on the cardiovascular system during daily activities.
What are the best types of exercises to mitigate heart disease risk?
Aerobic exercise provides the greatest benefits for heart health. Aerobic exercise in particular can improve circulation, reduce heart disease factors, and strengthen the heart and cardiovascular system.
Walking, swimming, cycling, and jogging are excellent cardiovascular exercises. These activities increase heart rate and improve blood flow throughout the body.
Strength training also supports heart health when combined with aerobic activity. It helps control blood pressure and improves overall fitness levels.
What is the relationship between a sedentary lifestyle and increased risk of coronary heart disease?
An inactive lifestyle is a risk factor for coronary heart disease. People who sit for long periods without regular movement face higher cardiovascular risks.
Sedentary behavior contributes to multiple heart disease risk factors. These include high blood pressure, elevated cholesterol levels, and increased body weight.
The combination of inactivity with other risk factors creates even greater danger. Smoking, poor diet, and lack of exercise together significantly increase heart attack and stroke risk.
How much should one exercise per week to effectively reduce heart disease risk?
Adults need at least 150 minutes of moderate-intensity exercise weekly. Adults should aim for at least 150 minutes a week of moderate-intensity physical activity such as brisk walking.
Alternatively, 75 minutes of vigorous activity per week provides similar benefits. 75 minutes of vigorous-intensity physical activity such as jogging meets the minimum requirements.
A combination of moderate and vigorous exercise also works effectively. This approach allows flexibility in meeting weekly activity goals.
What examples of moderate-intensity exercises can be done at home to prevent cardiovascular disease?
Brisk walking around the neighborhood counts as moderate-intensity exercise. This activity requires no special equipment and fits into most daily schedules.
Dancing, climbing stairs, and doing household chores like vacuuming provide cardiovascular benefits. These activities raise heart rate while accomplishing daily tasks.
Bodyweight exercises like jumping jacks, step-ups, and marching in place work well indoors. These movements can be done in small spaces without equipment.
Does the risk of heart disease vary by age in relation to exercise, and what are the age-specific exercise recommendations?
Most people who die of coronary heart disease are 65 or older. Age increases heart disease risk, making exercise more important as people get older.
The basic exercise guidelines remain consistent across adult age groups. However, the risk of heart problems due to physical activity is related to your fitness level rather than age alone.
Older adults may need to start with lighter activities and gradually increase intensity. People with existing health conditions should consult healthcare providers before beginning new exercise programs.